Production of Biosimilar Ustekinumab In CHO Cells
PIPPIG; Susanne ; et al.
U.S. patent application number 16/322846 was filed with the patent office on 2020-11-05 for production of biosimilar ustekinumab in cho cells. The applicant listed for this patent is FYB 202 PROJECT GMBH. Invention is credited to Carsten BROCKMEYER, Susanne PIPPIG.
| Application Number | 20200347126 16/322846 |
| Document ID | / |
| Family ID | 1000005015609 |
| Filed Date | 2020-11-05 |

| United States Patent Application | 20200347126 |
| Kind Code | A1 |
| PIPPIG; Susanne ; et al. | November 5, 2020 |
Production of Biosimilar Ustekinumab In CHO Cells
Abstract
The present invention relates to a method for producing an ustekinumab antibody in CHO cells. It further relates to the use of the produced antibody in the treatment of plaque psoriasis, psoriatic arthritis and inflammatory bowel disease.
| Inventors: | PIPPIG; Susanne; (Munich, DE) ; BROCKMEYER; Carsten; (Marzling, DE) | ||||||||||
| Applicant: |
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Family ID: | 1000005015609 | ||||||||||
| Appl. No.: | 16/322846 | ||||||||||
| Filed: | August 2, 2017 | ||||||||||
| PCT Filed: | August 2, 2017 | ||||||||||
| PCT NO: | PCT/EP2017/069522 | ||||||||||
| 371 Date: | February 1, 2019 |
| Current U.S. Class: | 1/1 |
| Current CPC Class: | C07K 2317/14 20130101; A61K 47/183 20130101; A61K 2039/54 20130101; C07K 2317/21 20130101; A61K 47/26 20130101; A61K 47/22 20130101; C07K 16/244 20130101; C07K 2317/41 20130101; C07K 2317/92 20130101; A61K 9/0019 20130101; C07K 2317/76 20130101; A61K 47/20 20130101 |
| International Class: | C07K 16/24 20060101 C07K016/24; A61K 47/22 20060101 A61K047/22; A61K 47/26 20060101 A61K047/26; A61K 9/00 20060101 A61K009/00; A61K 47/18 20060101 A61K047/18; A61K 47/20 20060101 A61K047/20 |
Foreign Application Data
| Date | Code | Application Number |
|---|---|---|
| Aug 3, 2016 | EP | 16182661.5 |
Claims
1. A method of producing a recombinant ustekinumab antibody drug product comprising the heavy chain and the light chain of ustekinumab, wherein the heavy chain has the sequence according to SEQ ID No. 1 and the light chain has the sequence according to SEQ ID No. 2 and wherein the heavy chain and the light chain together form the recombinant ustekinumab antibody, the method comprising: a) culturing Chinese Hamster Ovary (CHO) host cells, genetically modified to express the heavy chain and the light chain of ustekinumab, in a suitable culture medium under conditions that allow the cells to express the heavy chain and the light chain and to form the recombinant ustekinumab antibody; b) harvesting the recombinant ustekinumab antibody from the host cell culture to obtain a recombinant ustekinumab antibody preparation; c) optionally purifying the recombinant ustekinumab antibody preparation obtained in step b) by one or more purification step(s); d) determining that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation obtained in step b) or c) meets one or more of the following criteria (i) to (iv): (i) binding to IL-23 differs from that of the reference product by not more than 10%; (ii) binding to IL-12 differs from that of the reference product by not more than 20%; (iii) binding to FcRn differs from that of the reference product by less than 10%; and (iv) inhibition of IL12- and/or IL23-induced target gene expression differs from that of the reference product by not more than 20%; and e) combining the recombinant ustekinumab antibody from the recombinant ustekinumab antibody preparation with one or more pharmaceutically acceptable excipients to obtain the recombinant ustekinumab antibody drug product.
2. The method according to claim 1, wherein the IL12- and/or IL23 target gene is interferon gamma.
3. The method according to claim 1, wherein in step d) it is determined that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation meets all criteria (i) to (iv).
4. The method according to claim 1, wherein the binding to IL-23, IL-12 and/or FcRn or the expression of the target gene is determined by ELISA or bio-layer interferometry.
5. The method according to claim 1, wherein in step d) it is further determined that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation meets one or more of the following criteria (v) to (viii): (v) sialic acid content .ltoreq.5%, (vi) >90% of the sialic acid being N-acetylneuraminic acid, (vii) <10% of the sialic acid being N-glycolylneuraminic acid, and (viii) <50% of the recombinant ustekinumab antibody molecules comprise a C-terminal lysine.
6. The method according to claim 1, wherein in step d) it is further determined that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation meets one or more of the following criteria (ix) to (xi): (ix) content of galactosylated glycoforms of at least 30%; (x) content of afucosylated glycoforms of less than 8%; and (xi) content of high mannose glycoforms of less than 3%.
7. The method according to claim 1, wherein the CHO host cells are CHO-K1 cells or cells derived therefrom.
8. The method according to claim 1, wherein the CHO host cells are cultured in fed-batch mode.
9. The method according to claim 1, wherein the recombinant ustekinumab antibody drug product is produced in large scale.
10. The method according to claim 1, wherein the one or more pharmaceutically acceptable excipient(s) is/are selected from the group consisting of sucrose, L-histidine, L-histidine monohydrochloride monohydrate and polysorbate 80.
11. The method according to claim 10, wherein the recombinant ustekinumab antibody drug product comprises 90 mg/mL recombinant ustekinumab antibody, 1 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.04 mg/mL polysorbate 80, 76 mg/mL sucrose and water for injection.
12. A method for treating plaque psoriasis or psoriatic arthritis comprising administering the recombinant ustekinumab antibody drug product produced by the method of claim 1 to a patient in need thereof.
13. The method according to claim 1, wherein the one or more pharmaceutically acceptable excipient(s) is/are selected from the group consisting of sucrose, L-histidine, L-histidine monohydrochloride monohydrate, EDTA disodium salt dihydrate, methionine and polysorbate 80.
14. The method according to claim 13, wherein the recombinant ustekinumab antibody drug product comprises 5 mg/mL recombinant ustekinumab antibody, 1.8 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.4 mg/mL polysorbate 80, 85 mg/mL sucrose, 0.02 mg/ml EDTA disodium salt dehydrate, 0.4 mg/ml methionine and water for injection.
15. A method for treating Crohn's disease comprising administering the recombinant ustekinumab antibody drug product produced by the method of claim 1 to a patient in need thereof.
Description
FIELD OF THE INVENTION
[0001] The present invention relates to a method for producing an ustekinumab antibody in CHO cells. It further relates to the use of the produced antibody in the treatment of plaque psoriasis, psoriatic arthritis and inflammatory bowel disease.
BACKGROUND OF THE INVENTION
[0002] Ustekinumab which is marketed under the name Stelara.RTM. is a fully human IgG1.kappa. antibody which binds to the common p40 subunit of the cytokines IL-12 and IL-23. The antibody-bound cytokines can no longer bind to their cognate receptors and are therefore not able to elicit an inflammatory response in a patient's body. In Europe ustekinumab has received a marketing authorization for the treatment of moderate to severe plaque psoriasis and active psoriatic arthritis as well as for the treatment of moderately to severely active Crohn's disease.
[0003] Stelara.RTM. (ustekinumab) is expressed in a Sp2/0 murine myeloma cell line using a protein-free, chemically defined cell culture medium and purified by a series of affinity and ion exchange chromatographic steps and viral inactivation steps.
[0004] A biosimilar therapeutic antibody is a therapeutic antibody which is marketed after patent and data protection for the original product (also referred to as reference product) has expired and which has the same amino acid sequence as the original product, but may slightly differ in posttranslational modifications due to the use of another production process. Nevertheless, the biosimilar therapeutic antibody has to show a similar safety and efficacy profile as the reference product. In terms of safety the content of N-glycolylneuraminic acid (NGNA) and .alpha.1,3-galactose are important parameters, since these elements are potentially immunogenic and can cause hypersensitivity reactions (Chung et al. (2008) N. Engl. J. Med. 358: 1109-1117; Padler-Karavani et al. (2008) Glycobiology 18: 818-830). With respect to efficacy the binding of the antibody to its target and the Fc-mediated activity are important parameters. Further, the binding of the antibody to FcRn may influence the pharmacokinetic behaviour of the antibody.
[0005] The mouse Sp2/0 cells used in the production of the ustekinumab reference product produce a lower titer of the recombinant protein than the CHO cells. On the other hand, mouse cells are known to produce highly sialylated proteins and it is known that a human anti-IL12/IL23 antibody produced in SP2/0 cells has a high sialic acid content (Raju and Jordan (2012) mAbs 4:3, 385-391; Yu et al. (2016) Scientific Reports 7: 20029). According to the scientific literature the sialic acid content influences the target binding and the Fc mediated activity of antibodies (Scallon et al. (2007) Mol. Immunol. 44: 1524-1534; Kaneko et al. (2006) Science 313: 670-673).
[0006] WO 2012/012271 A1 and Dumont et al. (2016) Crit. Rev. Biotechnol. 36(6): 1110-1122 disclose that ustekinumab is produced in CHO cells. The Master thesis of Linda Schwaigerlehner ("Antibody gene expression in CHO cells with recombinase mediated cassette exchange") submitted in November 2015 and EP 3 059 319 A1 describe the production of ustekinumab in CHO cells, but do not provide any analysis of the produced antibody with respect to sialylation and activity.
[0007] Nevertheless, it was believed that a biosimilar ustekinumab has to be produced in the Sp2/0 cells to exert the same functions as the reference ustekinumab product.
SUMMARY OF THE INVENTION
[0008] The present inventors have surprisingly found that an ustekinumab antibody produced in CHO cells having a low sialic acid content shows essentially the same biological activity as the ustekinumab reference antibody.
[0009] Accordingly, the present invention relates to a method of producing a recombinant ustekinumab antibody drug product comprising the heavy chain and the light chain of ustekinumab, wherein the heavy chain has the sequence according to SEQ ID No. 1 and the light chain has the sequence according to SEQ ID No. 2 and wherein the heavy chain and the light chain together form the recombinant ustekinumab antibody, the method comprising: [0010] a) culturing Chinese Hamster Ovary (CHO) host cells, genetically engineered to express the heavy chain and the light chain of ustekinumab, in a suitable culture medium under conditions that allow the cells to express the heavy chain and the light chain and to form the recombinant ustekinumab antibody; [0011] b) harvesting the recombinant ustekinumab antibody from the host cell culture to obtain a recombinant ustekinumab antibody preparation; [0012] c) optionally purifying the recombinant ustekinumab antibody preparation obtained in step b) by one or more purification step(s); [0013] d) determining that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation obtained in step b) or c) meets one or more of the following criteria (i) to (iv): [0014] (i) binding to IL-23 differs from that of the reference product by not more than 10%; [0015] (ii) binding to IL-12 differs from that of the reference product by not more than 20%; [0016] (iii) binding to FcRn differs from that of the reference product by less than 10%; and [0017] (iv) inhibition of IL12- and/or IL23-induced target gene expression differs from that of the reference product by not more than 20%; and [0018] e) combining the recombinant ustekinumab antibody from the recombinant ustekinumab antibody preparation with one or more pharmaceutically acceptable excipients to obtain the recombinant ustekinumab antibody drug product.
[0019] Preferably, the IL12 and/or IL23 target gene is interferon gamma.
[0020] The binding to IL-23, IL-12 and/or FcRn or the expression of the target gene may be determined by ELISA or bio-layer interferometry.
[0021] Preferably, in step d) it is determined that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation meets all criteria (i) to (iv).
[0022] In one embodiment in step d) it is further determined that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation meets one or more of the following criteria (v) to (viii): [0023] (v) sialic acid content .ltoreq.5%, [0024] (vi) >90% of the sialic acid being N-acetylneuraminic acid, [0025] (vii)<10% of the sialic acid being N-glycolylneuraminic acid, and [0026] (viii)<50% of the recombinant ustekinumab antibody molecules comprise a C-terminal lysine.
[0027] In one embodiment in step d) it is further determined that the recombinant ustekinumab antibody in the recombinant ustekinumab antibody preparation meets one or more of the following criteria (ix) to (xi): [0028] (ix) content of galactosylated glycoforms of at least 30%; [0029] (x) content of afucosylated glycoforms of less than 8%; and [0030] (xi) content of high mannose glycoforms of less than 3%.
[0031] The CHO host cells may be CHO-K1 cells or cells derived therefrom.
[0032] The CHO host cells may be cultured in fed-batch mode.
[0033] The recombinant ustekinumab antibody drug product may be produced in large scale.
[0034] In one embodiment the one or more pharmaceutically acceptable excipient(s) is/are selected from the group consisting of sucrose, L-histidine, L-histidine monohydrochloride monohydrate and polysorbate 80.
[0035] Preferably, the recombinant ustekinumab antibody drug product comprises 90 mg/mL recombinant ustekinumab antibody, 1 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.04 mg/mL polysorbate 80, 76 mg/mL sucrose and water for injection.
[0036] The recombinant ustekinumab antibody drug product produced according to the method described herein may be used in treating plaque psoriasis or psoriatic arthritis.
[0037] In one embodiment the one or more pharmaceutically acceptable excipient(s) is/are selected from the group consisting of sucrose, L-histidine, L-histidine monohydrochloride monohydrate, EDTA disodium salt dihydrate, methionine and polysorbate 80.
[0038] Preferably, the recombinant ustekinumab antibody drug product comprises 5 mg/mL recombinant ustekinumab antibody, 1.8 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.4 mg/mL polysorbate 80, 85 mg/mL sucrose, 0.02 mg/ml EDTA disodium salt dehydrate, 0.4 mg/ml methionine and water for injection.
[0039] The recombinant ustekinumab antibody drug product produced according to the method described herein may be used in treating Crohn's disease.
DETAILED DESCRIPTION OF THE INVENTION
[0040] The present invention as illustratively described in the following may suitably be practiced in the absence of any element or elements, limitation or limitations, not specifically disclosed herein.
[0041] The present invention will be described with respect to particular embodiments, but the invention is not limited thereto, but only by the claims.
[0042] Where the term "comprising" is used in the present description and claims, it does not exclude other elements. For the purposes of the present invention, the term "consisting of" is considered to be a preferred embodiment of the term "comprising". If hereinafter a group is defined to comprise at least a certain number of embodiments, this is also to be understood to disclose a group which preferably consists only of these embodiments.
[0043] Where an indefinite or definite article is used when referring to a singular noun, e.g. "a", "an" or "the", this includes a plural of that noun unless something else is specifically stated.
[0044] Within the meaning of the present invention the term "composition" is to be understood in its broadest sense and refers to any composition in which the ustekinumab antibody is stable for at least some hours. Accordingly, the term composition includes cell culture media into which the ustekinumab antibody has been secreted, buffered salt solutions which result from one or more purification steps and pharmaceutical compositions which are intended to be administered to a patient. The composition typically comprises a mixture of several ustekinumab antibody molecules wherein the single antibody molecules may differ from each other in their glycosylation and charge due to a different degree of sialylation and the presence or absence of C-terminal lysine residues.
[0045] The term "antibody preparation" refers to a composition comprising the ustekinumab antibody which has been harvested from the host cell culture or to a composition which has been purified by one or more chromatographic steps. It does not refer to a composition which comprises the antibody and one or more pharmaceutically acceptable excipients.
[0046] The term "antibody drug product" refers to a composition which is ready to be administered to a patient for treating a disease. Accordingly, the antibody drug product comprises the antibody and one or more pharmaceutically acceptable excipients. As used herein, the term "antibody drug product" is equivalent to the term "pharmaceutical composition".
[0047] Ustekinumab which is marketed under the name Stelara.RTM. is a fully human IgG1.kappa. antibody which binds to the p40 subunit of both IL-12 and IL-23 and thereby blocks the inflammatory response in a patient's body. The amino acid sequences of the heavy and light chain of ustekinumab are displayed in SEQ ID Nos. 1 and 2 herein. In Europe ustekinumab has received a marketing authorization for the treatment of moderate to severe plaque psoriasis and of active psoriatic arthritis as well as for the treatment of moderately to severely active Crohn's disease.
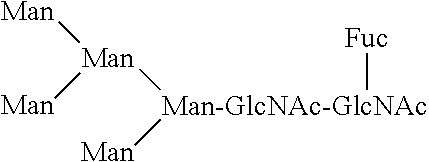
[0048] The ustekinumab antibody is glycosylated on the asparagine residue 299 of the Fc region of the antibody. The glycan attached to the Fc region via said asparagine residue has the following general formula:
##STR00001##
[0049] wherein GlcNAc refers to N-acetylglucosamine, Fuc refers to fucose, Gal.beta. refers to a galactose residue which is .beta.1,4-linked to an N-acetylglucosamine residue, Gal.alpha. refers to a galactose residue which is .alpha.1,3-linked to galactose, NeuGc refers to sialic acid and Man refers to mannose.
[0050] The glycoform wherein k, l and m in the above formula are each 0 is called the G0F glycoform. In addition, the antibody may be in the afucosylated form lacking the fucose attached to the N-acetylglucosamine. In this case the glycoform is denoted as G0.
[0051] To one or both terminal N-acetylglucosamine residues a galactose residue may be attached so that in this case k in the above formula is 1 or 2. The glycoform with one galactose residue (k=1 in the above formula) is called G1F (or G1 in case the fucose is not present) and the glycoform with two galactose residues (k=2 in the above formula) is called G2F (or G2 in case the fucose is not present).
[0052] Further, sialic acid residues may be attached to one or both galactose residues of the G1F/G1 or G2F/G2 structures so that in this case m in the above formula is 1 or 2 and 1 is 0 or 1. Instead of the one or two sialic acid residues one or two .alpha.-galactose residues may be linked to the terminal galactose, resulting in a terminal Gal-.alpha.1,3-Gal linkage (1 in the above formula is 1 or 2 and m is 0).
[0053] As discussed above, the ustekinumab antibody which is produced by the method of the present invention has a low sialic acid content. In particular, the sialic acid content of the ustekinumab antibody which is produced by the method of the present invention is significantly lower than the sialic acid content of the ustekinumab antibody produced in mouse cells, such as Sp2/0 cells.
[0054] Additionally, a glycoform may be present in which additional mannose residues are added to the mannose residues in the structure above so that the glycoform has the following structure:
##STR00002##
[0055] wherein GlcNAc refers to N-acetylglucosamine, Fuc refers to fucose and Man refers to mannose. This glycoform is also called Man5 or M5.
[0056] Within the meaning of the present invention the term "reference product" is used to denote the product with which the biosimilar product is compared to show similarity and bioequivalence. The reference product is therefore the product which has already obtained marketing approval. In the case of ustekinumab, the reference product is the approved Stelara.RTM. product or the ustekinumab antibody as present in the approved Stelara.RTM. product, respectively. For determining the similarity in the glycosylation between the reference product and the biosimilar, the ustekinumab antibody as present in the approved Stelara.RTM. product is used. The ustekinumab antibody is described in WO 2002/012500 A2.
[0057] "Sialic acid" is used to denote a group of compounds which are derivatives of the nine-carbon sugar neuraminic acid. The most common sialic acid forms in recombinant proteins are N-acetylneuraminic acid (NANA) and N-glycolylneuraminic acid (NGNA).
[0058] The term "sialic acid content" refers to the percentage of sialylated N-glycans in relation to the total amount of N-glycans in the glycoproteins within the composition. These glycoproteins are typically a mixture of glycoproteins with different glycan structures such as the G1F glycoform with one sialic acid molecule attached and the G2F glycoform with one or two sialic acid molecules attached.
[0059] The sialic acid content of the ustekinumab antibody which is produced by the method of the present invention is between 0 and 9%, preferably between 0.1 and 7% or between 0.1 and 5%, more preferably between 0.1 and 4% or between 0.1 and 3% or between 0.2 and 2.5%, even more preferably between 0.2 and 2% or between 0.2 and 1.8% and most preferably it is between 0.2 and 1.5% or between 0.2 and 1.4%.
[0060] For determining the sialic acid content the N-linked glycans are first released from the antibody by enzymatic reaction using a glycosidase such as PNGase F or PNGase A and then separated from the protein. Afterwards, the N-linked glycans are labelled with a suitable label including, but not being limited to, 2-AB (2-aminobenzamide), 2-AA (2-aminobenzoic acid), PA (2-aminopyridine), ANTS (2-aminonaphthalene trisulfonic acid), APTS (1-aminopyrene-3,6,8-trisulfonic acid) and RapiFluor-MS.TM. reagent. Suitable labelling kits are commercially available, for example the GlycoProfile.TM. 2-AB Labeling Kit of Sigma Aldrich, the Signal.TM. 2-AB Labeling Kit of ProZyme and the GlycoWorks RapiFluor-MS N-Glycan kit of Waters. Preferably, 2-AB or RapiFluor-MS.TM. reagent are used for labelling. The identification of glycans by labelling and subsequent detection is described in detail in Ruhaak et al. (2010) Anal. Bioanal. Chem. 397: 3457-3481.
[0061] After purification of the labelled N-linked glycans from the excess reagent they are separated and detected by a suitable method such as hydrophilic interaction liquid chromatography (HILIC), gel permeation chromatography or gas chromatography. Preferably, HILIC is used for separating and detecting N-linked glycans. Suitable stationary phases comprise amine-bonded silica, amide-bonded silica, ZIC HILIC phases and diol phases. Suitable columns are commercially available, such as the Xbridge Glycan BEH Amide XP Column (130 .ANG., 2.5 .mu.m, 2.1 mm.times.150 mm) of Waters. Suitable mobile phases comprise water in acetonitrile with a low concentration of acid or salt. Preferably, 50-100 mM ammonium formate in acetonitrile is used.
[0062] The sample comprising the N-linked glycans may be applied to the column in 50% acetonitrile and may be eluted from the column by increasing the percentage of ammonium formate in the solution. The peaks corresponding to the specific N-glycans, in particular the sialylated N-glycans, can be identified by comparison to the peaks of a standard or by mass spectrometry. The mass spectrometry also allows to distinguish between NGNA- and NANA-sialylated glycans. The sialic acid content is calculated as the percentage of the area of the peaks of all sialylated glycoforms in relation to the area of the peaks of all glycoforms within the sample.
[0063] The sialic acid present in the ustekinumab antibody of the present invention is predominantly N-acetylneuraminic acid (NANA), i.e. at least 90% or 91%, preferably at least 92% or 93%, more preferably at least 94% or 95%, even more preferably at least 96% or 97% and most preferably at least 98% or 99% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NANA.
[0064] The NANA content can also be determined using commercially available kits (e.g. Sialic Acid (NANA) Assay Kit ab83375 of abcam; Sialic Acid Quantitation Kit of Sigma-Aldrich) which measure the NANA content after its release from glycoproteins by enzymatic digestion using neuraminidase or acid hydrolysis. The released NANA can then be detected for example by an enzyme-coupled reaction in which free sialic acid is oxidized to an intermediate which then reacts with a probe to a product which can be detected by absorbance or fluorescence. Alternatively, the released NANA can be labeled with the fluorescent agent DMB (4,5-methylene-dioxy-1,2-phenylenediamine dihydrochloride) and detected by RP-HPLC. As described above, the NANA content can also be determined by mass spectrometry.
[0065] The ustekinumab antibody which is produced by the method of the present invention contains only low amounts of N-glycolylneuraminic acid (NGNA), i.e. less than 10% or 9%, preferably less than 8% or 7%, more preferably less than 6% or 5%, even more preferably less than 4% or 3% and most preferably less than 2% or 1% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NGNA. NGNA can be detected and quantified using NGNA-specific antibodies (see, e.g., Diaz et al. (2009) PloS ONE 4(1): e4241). As described above, the NGNA content can also be determined by mass spectrometry.
[0066] The content of NANA and NGNA can also be determined using high-performance anion-exchange chromatography with pulsed amperometric detection (HPAEC-PAD) which additionally allows to distinguish between NANA and NGNA (Rohrer et al. (1998) Glycobiol. 8(1): 35-43). The sialic acid species which is attached to sialylated N-glycans can also be determined using liquid chromatography, a mass detector and the GlycoWorks RapiFluor-MS N-Glycan kit of Waters.
[0067] In the ustekinumab antibody which is produced by the method of the present invention at least 90% or 91% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NANA and less than 10% or 9% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NGNA, preferably at least 92% or 93% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NANA and less than 8% or 7% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NGNA, more preferably at least 94% or 95% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NANA and less than 6% or 5% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NGNA, even more preferably at least 96% or 97% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NANA and less than 4% or 3% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NGNA and most preferably at least 98% or 99% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NANA and less than 2% or 1% of all sialic acids attached to the ustekinumab antibody produced by the method of the present invention are NGNA.
[0068] The inventors have further observed that the ustekinumab antibody produced by the method of the present invention has a lower amount of terminal .alpha.-galactose, which is linked to the terminal galactose of the G1/G1F or G2/G2F glycoforms by an .alpha.1,3-linkage, than in the reference product. Thus, the content of terminal .alpha.-galactose as defined above is less than or equal to 0.1%. The content of terminal .alpha.-galactose can be determined as described above for the sialic acid content.
[0069] The composition produced by the method of the present invention also differs from the reference product marketed as Stelara.RTM. in the distribution of the G0F and G2F glycoforms. The content of the G0F glycoform is at least 35%, preferably at least 40% or 42%, more preferably at least 45% or 48% and most preferably at least 50%. The content of the G0F glycoform is between 35% and 70%, preferably between 40% or 42% and 70%, more preferably between 45% or 48% and 68% and most preferably between 50% and 68% or between 55% and 65%. The content of the G2F glycoform is less than 6.5%, preferably less than 6.2%, more preferably less than 6% and most preferably less than 5.8%. The content of the G2F glycoform is between 1.5% and 6.5%, preferably between 1.8% or 2% and 6.2%, more preferably between 2.2% and 6% and most preferably between 2.4% and 5.8%.
[0070] The content of the G0F glycoform is at least 35% and the content of the G2F glycoform is less than 6.5%. Preferably, the content of the G0F glycoform is at least 40% or 42% and the content of the G2F glycoform is less than 6.2%. More preferably, the content of the G0F glycoform is at least 45% or 48% and the content of the G2F glycoform is less than 6%. Most preferably, the content of the G0F glycoform is at least 50% and the content of the G2F glycoform is less than 5.8%. The content of the G0F glycoform is between 35% and 70% and the content of the G2F glycoform is between 1.5% and 6.5%. Preferably, the content of the G0F glycoform is between 40% or 42% and 70% and the content of the G2F glycoform is between 1.8% or 2% and 6.2%. More preferably, the content of the G0F glycoform is between 45% or 48% and 68% and the content of the G2F glycoform is between 2.2% and 6%. Most preferably, the content of the G0F glycoform is between 50% and 68% or between 55% and 65% and the content of the G2F glycoform is between 2.4% and 5.8%.
[0071] The content of the G0F and G2F glycoforms can be determined as described above for the sialic acid content.
[0072] The ustekinumab antibody produced by the method of the present invention has a content of galactosylated glycoforms of at least 30%, preferably of at least 32%, more preferably of at least 34% and most preferably of at least 35%. The ustekinumab antibody produced by the method of the present invention has a content of galactosylated glycoforms of between 25% and 50%, preferably of between 30% and 45%, more preferably of between 32% and 42% and most preferably of between 33% and 40%. The content of galactosylated glycoforms can be determined by calculating the sum of the percentages of glycoforms having at least one galactose residue, i.e. glycoforms G1F, G1, G2 and G2F.
[0073] The ustekinumab antibody produced by the method of the present invention has a content of afucosylated glycoforms of less than 8%, preferably less than 7%, more preferably less than 6% and most preferably of less than 5%. The ustekinumab antibody produced by the method of the present invention has a content of afucosylated glycoforms of between 0.5% to 8%, preferably between 0.8% and 7%, more preferably between 1% and 6% and most preferably between 1.5% and 4%. The content of afucosylated glycoforms can be determined by calculating the sum of the percentages of glycoforms which do not comprise at least one fucose.
[0074] The ustekinumab antibody produced by the method of the present invention has a content of high mannose (M5) glycoforms of less than 3%, preferably of less than 2.5%, more preferably less than 2.2% and most preferably of less than 1.8%. The ustekinumab antibody produced by the method of the present invention has a content of high mannose (M5) glycoforms of between 0.1% and 3%, preferably between 0.2% and 2.5%, more preferably between 0.3% and 2.2% and most preferably between 0.4% and 1.8%. The content of the high mannose glycoform can be determined as described above for the sialic acid content.
[0075] Another difference between the ustekinumab antibody produced by the method of the present invention and the antibody present in the reference product marketed as Stelara.RTM. as well as an antibody produced in Sp2/0 cells is the percentage of antibody molecules having a C-terminal lysine residue. The term "C-terminal lysine residue" refers to the lysine residue which is located on the C-terminus of the IgG1 heavy chain constant region and therefore terminates the CH3 domain of the heavy chain constant region.
[0076] At least 50% of the ustekinumab molecules produced by the method of the present invention do not comprise a C-terminal lysine residue. Preferably at least 53% or 56%, more preferably at least 58% or 60% and most preferably at least 63% of the ustekinumab molecules produced by the method of the present invention do not comprise a C-terminal lysine residue. Further, from 50 to 75% of the ustekinumab molecules do not comprise a C-terminal lysine residue. Preferably, 52% to 74% or 55% to 73%, more preferably 57% to 72% or 60% to 71% and most preferably 63% to 70% of the ustekinumab molecules produced by the method of the present invention do not comprise a C-terminal lysine residue. These numbers refer to the main peak of the protein having no C-terminal lysine residue as obtained by cation exchange chromatography.
[0077] The percentage of antibody molecules which comprise no, one or two C-terminal lysine residues can be determined by any suitable method including cation exchange chromatography (CEX), isoelectric focusing (IEF), capillary zone electrophoresis (CZE), capillary isoelectric focusing (cIEF) and liquid chromatography-mass spectrometry (LC-MS), preferably it is determined using cation exchange chromatography. For example, a sample of the antibody may be loaded onto a weak cation exchange chromatography column having carboxyl groups as functional groups in a solution containing 20 mM sodium phosphate buffer, pH 7.5 and the antibody may be eluted by sequentially increasing the percentage of a salt-containing buffer such as 20 mM sodium phosphate buffer, pH 7.5 and 25 mM NaCl. The peaks corresponding to proteins with no, one or two C-terminal lysine residues can be identified by treatment with specific enzymes or mass spectrometry. The percentage of antibody molecules which do not comprise a C-terminal lysine residue can be calculated as the ratio of the peak area for the isoform having no lysine residue to the total peak area. The above percentage is calculated using the main peak representing the protein with no C-terminal lysine residue as obtained by cation exchange chromatography performed as described above and in the examples section.
[0078] As discussed before, the present inventors have surprisingly found that despite the lower sialic acid content the ustekinumab antibody which is produced by the method of the present invention essentially has the same biological activity as the reference product Stelara.RTM. and an ustekinumab antibody produced in mouse cells. The biological activity of the ustekinumab antibody includes one or more of binding to IL-23, binding to IL-12, binding to FcRn and inhibition of IL12-induced gene expression.
[0079] The binding of the antibody to IL-23, IL-12 or FcRn may be assessed using methods including, but not being limited to, ELISA and bio-layer interferometry.
[0080] The skilled person is aware of protocols for performing an ELISA assay. In brief, the target of the antibody, i.e. IL-12 or IL-23 in case of ustekinumab, is coated onto a plate, incubated with the ustekinumab antibody, washed and then the bound antibody is detected and quantified with a labelled antibody specific for human IgG.
[0081] Bio-layer interferometry is a label-free optical analytical technique which analyzes the interference pattern of white light reflected from two surfaces, i.e. a layer of immobilized protein on the biosensor tip and an internal reference layer. The binding of molecules to the biosensor tip, e.g. by interaction of an antibody with its cognate target, leads to a shift in the interference pattern that can be measured in real-time. For measuring the interaction between ustekinumab and its target the ustekinumab antibody is immobilized on the biosensor tip and contacted with a solution containing the target protein.
[0082] The binding of the ustekinumab antibody produced by the method of the present invention to IL-12 or IL-23 is essentially the same as that of the reference product, i.e. the binding to IL-12 or IL-23 differs by less than 20%, preferably by less than 15% from the binding of the reference product.
[0083] Surprisingly, it has been found that the binding of the ustekinumab antibody produced by the method of the present invention to IL-23 and IL-12 is similar to the binding of the reference product to IL-23 and IL-12.
[0084] The binding of the ustekinumab antibody produced by the method of the present invention to IL-23 differs by not more than 10%, preferably by not more than 9%, more preferably by not more than 8%, even more preferably by not more than 7% and most preferably by not more than 5% from the binding of the reference product to IL-23.
[0085] The binding of the ustekinumab antibody produced by the method of the present invention to IL-12 differs by not more than 20%, preferably by not more than 15%, more preferably by not more than 12% and most preferably by not more than 10% from the binding of the reference product to IL-12.
[0086] The binding of the ustekinumab antibody produced by the method of the present invention to FcRn is essentially the same as that of the reference product, i.e. the dissociation constant K.sub.D for binding to FcRn differs by less than 10%, preferably by less than 8%, more preferably by less than 6% and most preferably by less than 4% from the dissociation constant K.sub.D of the reference product.
[0087] The inhibition of IL12-induced gene expression by the ustekinumab antibody can for example be investigated by incubating cells which are responsive to IL-12, such as the human natural killer lymphoma cell line NK-92, with IL-12 and the antibody sample and then detecting the production of a target molecule, such as interferon-gamma (IFN-.gamma.). The target molecule, e.g. IFN.gamma., may be detected and/or quantified by any suitable method, such as ELISA.
[0088] Surprisingly, it has been found that the inhibition of IFN.gamma. production by the ustekinumab antibody produced by the method of the present invention is as strong as the inhibition of IFN.gamma. production by the reference product. The inhibition of IFN.gamma. production by the ustekinumab antibody produced by the method of the present invention differs by not more than 16%, preferably by not more than 14%, more preferably by not more than 12% and most preferably by not more from 10% from the inhibition of IFN.gamma. production by the reference product.
[0089] The method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets one or more of the following criteria (i) to (iv): [0090] (i) binding to IL-23 differs from that of the reference product by not more than 10%; [0091] (ii) binding to IL-12 differs from that of the reference product by not more than 20%; [0092] (iii) binding to FcRn differs from that of the reference product by less than 10%; and [0093] (iv) inhibition of IL12- and/or IL23-induced target gene expression differs from that of the reference product by not more than 20%.
[0094] Preferably, the target gene of IL12 and/or IL23 is interferon gamma.
[0095] In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets one of the above criteria (i) to (iv). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets two of the above criteria (i) to (iv), such as criteria (i) and (ii), (i) and (iii), (i) and (iv), (ii) and (iii), (ii) and (iv) or (iii) and (iv). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets three of the above criteria (i) to (iv), such as criteria (i), (ii) and (iii) or (ii), (iii) and (iv). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets all four of the above criteria (i) to (iv).
[0096] The determination whether the recombinant ustekinumab antibody preparation meets above criterion (i) comprises measuring the binding of the recombinant ustekinumab antibody preparation and the reference product to IL-23 and calculating the difference in binding. The determination whether the recombinant ustekinumab antibody preparation meets above criterion (ii) comprises measuring the binding of the recombinant ustekinumab antibody preparation and the reference product to IL-12 and calculating the difference in binding. The determination whether the recombinant ustekinumab antibody preparation meets above criterion (iii) comprises measuring the binding of the recombinant ustekinumab antibody preparation and the reference product to FcRn and calculating the percentage of different binding. The determination whether the recombinant ustekinumab antibody preparation meets above criterion (iv) comprises measuring the expression of a known target gene of IL12 and/or IL23 in cells treated with the recombinant ustekinumab antibody preparation or the reference product and calculating the difference in target gene expression. If the target gene is interferon gamma, the interferon gamma production in cells treated with the recombinant ustekinumab antibody preparation or the reference product is measured and the difference in interferon gamma production is calculated.
[0097] The method of the present invention may additionally comprise determining that the recombinant ustekinumab antibody preparation meets one or more of the following criteria (v) to (viii): [0098] (v) sialic acid content .ltoreq.5%, [0099] (vi) >90% of the sialic acid being N-acetylneuraminic acid, [0100] (vii) <10% of the sialic acid being N-glycolylneuraminic acid, and [0101] (viii) <50% of the recombinant ustekinumab antibody molecules comprise a C-terminal lysine.
[0102] In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets one of the above criteria (v) to (viii). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets two of the above criteria (v) to (viii), such as criteria (v) and (vi), (v) and (vii), (v) and (viii), (vi) and (vii), (vi) and (viii) or (vii) and (viii). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets three of the above criteria (vi) to (viii), such as criteria (v), (vi) and (vii) or (vi), (vii) and (viii). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets all four of the above criteria (v) to (viii).
[0103] The method of the present invention may additionally comprise determining that the recombinant ustekinumab antibody preparation meets one or more of the following criteria (ix) to (xi): [0104] (ix) content of galactosylated glycoforms of at least 30%; [0105] (x) content of afucosylated glycoforms of less than 8%; and [0106] (xi) content of high mannose glycoforms of less than 3%.
[0107] In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets one of the above criteria (ix) to (xi). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets two of the above criteria (ix) to (xi), such as criteria (ix) and (x), (ix) and (xi) or (x) and (xi). In one embodiment, the method of the present invention comprises determining that the recombinant ustekinumab antibody preparation meets all three of the above criteria (ix) to (xi).
[0108] As discussed above, according to the present invention the ustekinumab antibody is produced in CHO cells. CHO cells are epithelial cells which are derived from the ovary of the Chinese hamster ovary (Tijo and Puck (1958) J. Exp. Med. 108: 259-271). From the original CHO cell line several other cell lines have been obtained, including CHO-K1, CHO-Toronto, CHO-DXB11, CHO-DG44 and CHO K1 SV. All these cell lines can be used to produce the composition comprising ustekinumab according to the present invention.
[0109] Preferably, a CHO-K1 cell line or cells derived therefrom is used to produce the composition comprising ustekinumab of the present invention. The CHO-K1 cell line has been obtained from a single clone of the original CHO cells (Kao and Puck (1968) Proc. Nat. Acad. Sci. USA 60(4): 1275-1281). The CHO-K1 cell line can be adapted to suspension growth and/or to a chemically defined medium (see, e.g., Bort et al. (2010) Biotechnol. J. 5(10): 1090-1097). In the present invention preferably CHO-K1 cells or cells derived therefrom are used. The cells which are derived from the CHO-K1 cells are cells which originate from the CHO-K1 cells, but have been subjected to one or more adaptation processes, such as adaptation to serum-free medium or suspension growth.
[0110] The CHO cells used to produce the ustekinumab antibody have been genetically modified to express the ustekinumab antibody. The term "genetically modified CHO cells" as used herein means that CHO cells have been modified or altered by any suitable genetic means and methods known to the skilled person such that they express the ustekinumab antibody. In one embodiment, the genetic modification to express the ustekinumab antibody is the only genetic modification of the CHO cells. In another embodiment the CHO cells are genetically modified to increase or decrease the expression of one or more enzymes which have an impact on the sialic acid content of proteins, such as sialyltransferases or sialidases. In one embodiment, the CHO cells are genetically modified to decrease the expression of one or more sialidases. In another embodiment the CHO cells are genetically modified to increase the expression of one or more sialyltransferases. A CHO cell line which is genetically modified to express an .alpha.2,6-sialyltransferase is described in Onitsuka et al. (2012) Appl. Microbiol. Biotechnol. 94: 69-80. Preferably, the CHO cells do not comprise a genetic modification other than the genetic modification to express the ustekinumab antibody.
[0111] Methods for genetically modifying CHO cells are known to the skilled person and particularly include the transfection of the CHO cells with one expression vector encoding the heavy and the light chain of the antibody or with a first expression vector encoding the heavy chain of the antibody and a second expression vector encoding the light chain of the antibody. In one embodiment, the recombinant antibody is produced from one recombinant nucleic acid molecule which encodes both the heavy and the light chain of the antibody. In a more preferred embodiment, the recombinant antibody is produced from two recombinant nucleic acid molecules having the same or different promoters. In an even more preferred embodiment, the recombinant antibody is produced from two recombinant nucleic acid molecules having the same promoter. In a most preferred embodiment, the recombinant antibody is produced from two recombinant nucleic acid molecules which differ from each other only by the encoded gene and the selection marker used to select the transfected cells.
[0112] The elements and methods needed to construct expression vectors which are suitable for expressing an antibody in CHO cells are well-known to the skilled person and described for example in Makrides et al. (1999) Protein Expr. Purif. 17: 183-202 and Kaufman (2000) Mol. Biotechnol. 16: 151-161. Further, the skilled person is aware of methods for introducing the expression vectors into the CHO cells. These methods include the use of commercially available transfection kits such as Lipofectamine.RTM. of ThermoFisher, PElmax of Polyplus Sciences) or Freestyle Max of Invitrogen. Further suitable methods include electroporation, calcium phosphate-mediated transfection and DEAE-dextrane transfection. After transfection the cells are subjected to selection by treatment with a suitable agent based on the selection marker(s) encoded by the expression vector(s) to identify the stably transfected cells.
[0113] To produce the ustekinumab antibody the genetically modified CHO cells are cultured in a suitable culture medium. The terms "medium", "cell culture medium" and "culture medium" are interchangeably used herein and refer to a solution containing nutrients which are required for growing mammalian cells. Typically, a cell culture medium provides essential and non-essential amino acids, vitamins, energy sources, lipids, and trace elements required by the cell for minimal growth and/or survival. Preferably, the medium is chemically defined in that all its components and their concentration are known. Also preferably, the medium is serum-free and hydrolysate-free and does not contain any components derived from animals. More preferably, the medium is chemically defined, serum-free, animal-component-free and hydrolysate-free.
[0114] Media for growing CHO cells are commercially available and include PowerCHO-2 CD available from Lonza, CD OptiCHO.TM. Medium available from ThermoFisher and EX-CELL.RTM. CD CHO Serum-Free Medium available from Sigma-Aldrich. These media may be supplemented with further reagents such as recombinant insulin, lipids, ferric citrate, PEG20000, extra amounts of some sugar types and extra amounts of some or all amino acids.
[0115] Preferably, the CHO cells are cultured in suspension, i.e. in a non-adherent state.
[0116] The galactose content of the antibody may be increased by adding suitable amounts of galactose, manganese ions and/or uridine to the cell culture medium (Gramer et al. (2011) Biotechnol. Bioeng. 108(7): 1591-1602; WO 2012/149197 .ANG.2).
[0117] For culturing the CHO cells different strategies are available, including batch culture, continuous culture and fed-batch culture. Within the present invention, preferably a fed-batch culture process is used to produce ustekinumab. In fed-batch culture the culturing process is started with a certain volume of the medium and one or more nutrients are fed at later time-point(s) of the culture process to prevent nutrient depletion while no product is removed from the cell culture broth.
[0118] The method of the present invention may be used to produce ustekinumab in large scale, i.e. in a production volume of at least 501 or 1001, preferably of at least 5001 or at least 1.0001, more preferably of at least 5.0001 and most preferably of at least 10.0001 or 20.0001.
[0119] After the ustekinumab antibody has been produced by the CHO cells, it is harvested. Since recombinant proteins, in particular antibodies, expressed from mammalian cells are typically secreted into the cell culture fluid during the cultivation process, the product harvest at the end of the cultivation process occurs by separating cell culture fluid comprising the ustekinumab antibody from the cells. The cell separation method should be gentle to minimize cell disruption to avoid the increase of cell debris and release of proteases and other molecules that could affect the quality of the immunoglobulin product. Usually, the harvesting of the cell culture fluid comprising the ustekinumab involves centrifugation and/or filtration, whereby the recombinant protein is present in the supernatant and the filtrate, respectively. Expanded bed adsorption chromatography is an alternative method to avoid centrifugation/filtration methods.
[0120] After harvesting the cell culture fluid comprising the ustekinumab antibody, the antibody has to be purified from the cell culture fluid. The purification of recombinant proteins and in particular recombinant antibodies is usually accomplished by a series of chromatographic steps such as anion exchange chromatography, cation exchange chromatography, affinity chromatography, hydrophobic interaction chromatography, hydroxyapatite chromatography, mixed mode chromatography and size exclusion chromatography. The purification of recombinant antibodies usually starts with a protein A affinity chromatography to capture the antibody and is followed by one or more additional chromatographic steps such as cation exchange chromatography and mixed mode chromatography. Further, the purification process may comprise one or more ultra-, nano- or diafiltration steps.
[0121] Also described herein is a pharmaceutical composition comprising an ustekinumab antibody, wherein the antibody has a sialic acid content of 0 to 5%.
[0122] A pharmaceutical composition is a composition which is intended to be delivered to a patient for treating or preventing a disease or condition. In addition to the active agent, in the present case the ustekinumab antibody, a pharmaceutical composition also contains at least one pharmaceutically acceptable excipient. Pharmaceutically acceptable excipients are substances which do not interfere with the physiological activity of the active agent such as the ustekinumab antibody and which stabilize the pharmaceutical composition and/or enhance solubility or decrease viscosity of the pharmaceutical composition. Typical pharmaceutically acceptable excipients for monoclonal antibodies include buffers, salts, sugars or sugar alcohols, amino acids and surface-active agents.
[0123] The pharmaceutical composition preferably contains sucrose, L-histidine, L-histidine monohydrochloride monohydrate and polysorbate 80. More preferably, the pharmaceutical composition of the present invention contains 76 mg/mL sucrose, 1 mg/mL L-histidine/L-histidine monohydrochloride monohydrate and 0.04 mg/mL polysorbate 80 in water for injection (WFI). Most preferably, the pharmaceutical composition consists of 90 mg/mL ustekinumab antibody as characterized herein, 76 mg/mL sucrose, 1 mg/mL L-histidine, 1 mg/mL L-histidine monohydrochloride monohydrate and 0.04 mg/mL polysorbate 80 in water for injection (WFI).
[0124] The pharmaceutical composition described above can be used in the treatment of plaque psoriasis, in particular the treatment of moderate to severe plaque psoriasis in adults who failed to respond to, or who have a contraindication to, or are intolerant to other systemic therapies including cyclosporin, methotrexate (MTX) or PUVA (psoralen and ultraviolet A) and the treatment of moderate to severe plaque psoriasis in adolescent patients from the age of 12 years and older, who are inadequately controlled by, or are intolerant to, other systemic therapies or phototherapies and psoriatic arthritis, in particular the treatment of active psoriatic arthritis in adult patients when the response to previous non-biological disease-modifying anti-rheumatic drug (DMARD) therapy has been inadequate.
[0125] The pharmaceutical composition may also be used in the treatment of adult patients with moderate to severe plaque psoriasis (Ps) who are candidates for phototherapy or systemic therapy or for the treatment of active psoriatic arthritis (PsA), alone or in combination with methotrexate.
[0126] The recommended dosage of ustekinumab for the treatment of adult patients having plaque psoriasis or psoriatic arthritis is 45 mg or 90 mg, depending on the body weight, administered subcutaneously, followed by a 45 mg or 90 mg dose 4 weeks later, and then every 12 weeks thereafter.
[0127] In another embodiment the pharmaceutical composition contains sucrose, L-histidine, L-histidine monohydrochloride monohydrate, EDTA disodium salt dihydrate, methionine and polysorbate 80. More preferably, the pharmaceutical composition comprises 5 mg/mL recombinant ustekinumab antibody, 1.8 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.4 mg/mL polysorbate 80, 85 mg/mL sucrose, 0.02 mg/ml EDTA disodium salt dihydrate, 0.4 mg/ml methionine and water for injection. Most preferably, the pharmaceutical composition consists of 5 mg/mL recombinant ustekinumab antibody, 1.8 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.4 mg/mL polysorbate 80, 85 mg/mL sucrose, 0.02 mg/ml EDTA disodium salt dihydrate, 0.4 mg/ml methionine and water for injection.
[0128] This pharmaceutical composition can be used in the treatment of adult patients with moderately to severely active Crohn's disease who have had an inadequate response with, lost response to, or were intolerant to either conventional therapy or a TNF.alpha. antagonist or have medical contraindications to such therapies.
[0129] The recommended dosage of ustekinumab for the treatment of adult patients with moderately to severely active Crohn's disease is 260 mg to 520 mg, depending on the body weight, administered by intravenous injection using the above pharmaceutical composition containing sucrose, L-histidine, L-histidine monohydrochloride monohydrate, EDTA disodium salt dihydrate, methionine and polysorbate 80. After this initial intravenous injection the following doseis administered by subcutaneous injection using the above pharmaceutical composition containing sucrose, L-histidine, L-histidine monohydrochloride monohydrate and polysorbate 80. The subcutaneous injections start eight weeks after the intravenous injection. The recommended doses of ustekinumab for subcutaneous administration are 90 mg every 8 weeks following the first s.c. injection.
[0130] The following examples are provided for illustrative purposes. It is thus understood that the examples are not to be construed as limiting. The skilled person in the art will clearly be able to envisage further modifications of the principles laid out herein.
Examples
[0131] The present invention is supported and illustrated by reference to the following non-limiting examples.
[0132] 1. Production of the Ustekinumab Antibody in CHO Cells
[0133] CHO-K1 cells were transfected with a first expression vector expressing the heavy chain of ustekinumab under the control of a first promoter and additionally containing a first selection marker gene and a second expression vector expressing the light chain of ustekinumab under the control of said first promoter and additionally containing a second selection marker gene. Transfected cells were selected by treatment with substances matching to the selection marker genes and single clones of the CHO-K1 cells were obtained after some rounds of subculturing. The supernatant of these single clones was then purified by protein A chromatography and then subjected to glycoform characterisation and activity assays as described below.
[0134] 2. Glycoform Characterisation
[0135] 2.1 Sample Preparation
[0136] The protein sample was diluted with 5 mM Tris/HCl, pH 7.0 to a final concentration of 1.25 .mu.g/.mu.L. 1.5 .mu.l PNGase F and 2.5 .mu.L of 1.5% IGEPAL CA-630 were added to 120 .mu.L of the diluted sample for the deglycosylation reaction. This mixture was incubated for 17 hours at 37.degree. C., before the released N-glycans were purified from the protein by centrifugation with Amicon.RTM. Ultra-0.5 30K filter devices, wherein the filtrate contains the N-glycans. The filtrate was dried in a vacuum concentrator and then 10 .mu.L derivatization solution (0.5 M 2-AB in DMSO/acetic solution) and 10 reduction solution (1 M sodium cyanoborohydride in DMSO/acetic solution) were added and the mixture was incubated for 17 hours at 37.degree. C. The labelled N-glycans were purified from excess reagent by gel filtration using NAP-5 size exclusion columns. The flow-through of the column was collected, dried using a vacuum concentrator and the pellet was dissolved in 50% acetonitrile.
[0137] For identification of sialylated N-glycan peaks, the N-glycans were desialylated by mild acidic hydrolysis using 2 M acetic acid and incubation at 80.degree. C. for two hours.
[0138] The resulting sample was subjected to HPLC using the following settings:
[0139] Column: XBridge Glycan BEH Amide XP Column 130 .ANG., [0140] 2.5 .mu.m, 2.1 mm.times.150 mm
[0141] Column temperature: 60.degree. C.
[0142] Auto sampler temperature: 8.degree. C.
[0143] Injection volume: 2 .mu.L
[0144] Detection: FLD Ex 260 nm, .mu.m 428 nm
[0145] Mobile phase A: 100 mM ammonium formate in water, pH 5.0
[0146] Mobile phase B: Acetonitrile
[0147] Gradient:
TABLE-US-00001 Time Eluent B Flow rate [min] [% Acetonitrile] [mL/min] Parameter 0 72 0.34 Separation 70 50 0.34 73 20 0.17 Cleaning 83 20 0.17 85 72 0.17 Equilibration 95 72 0.17 100 72 0.34
[0148] The relative quantity of each N-glycan peak was calculated by comparing the area of a particular peak to the sum of all N-glycan peaks.
[0149] Table 1 shows the result of the glycoform analysis of three selected CHO subclones in comparison to three different batches of the reference product:
TABLE-US-00002 Sialo + Cell G0F G1F G2F .alpha.- line Description ID [%] [%] [%] gal [%] -- Reference 1 25.7 32.6 10.3 22.4 product -- Reference 2 25.3 33.9 8.8 23.4 product -- Reference 3 26.6 35.3 9.1 23.6 product CHO-K1 subclone 485-11#8 66.6 24.2 2.5 0.2 CHO-K1 subclone 567-7#54 58.4 28.2 3.9 0.9 CHO-K1 subclone 563-24#103 53.2 34.2 5.4 1.1
[0150] It is apparent from the above results that the CHO-produced antibody molecules produced by the method of the present invention have a significantly lower content of sialic acids than the reference product. Further, they have a higher percentage of the G0F glycoform and a lower content of the G2F glycoform than the reference product.
[0151] For distinguishing between NANA and NGNA the N-glycans were labelled with the GlycoWorks RapiFluor-MS Kit of Waters. After elimination of excessive reagent and protein by HILIC solid-phase extraction, the N-glycans were separated via HILIC-UPLC equipped with a fluorescence detector (Waters, FLR) and a mass detector (Waters, Acquity QDa). For fluorescence signals with a relative peak area of >0.1%, QDa data were evaluated in the scan range from 350-1250 m/z. The peaks corresponding to glycoforms containing NANA and NGNA were identified by comparison to known N-glycan masses from the NIBRT glycobase 3.2 database.
[0152] Table 2 shows the results of a representative sialic acid analysis for clone 485-11#8:
TABLE-US-00003 Reference product CHO-produced ustekinumab Total amount of glycoforms 0.5% 0.3% containing NANA Total amount of glycoforms 19.6% not detectable containing NGNA
[0153] This analysis shows that 100% of the sialic acid molecules present on the CHO-produced ustekinumab are NANA, whereas the reference product predominantly contains NGNA.
[0154] 3. Determination of Charge Heterogeneity
[0155] The protein sample was diluted with 20 mM sodium phosphate buffer pH 7.5 to 1 mg/mL. Sample was injected onto the cation exchange column and separated according to their charge heterogeneity. Charge isoforms were eluted in a salt gradient and detected using an UV detector at 214 nm.
[0156] The following settings were used for determining charge heterogeneities by cation exchange (CEX) HPLC:
[0157] Column Dionex, BioLCProPac.RTM. WCX-10, 4.0.times.250 mm, [0158] 10 .mu.m
[0159] Flow rate: 1.0 mL/min
[0160] Column temperature: 40.degree. C.
[0161] Autosampler temperature: 6.degree. C.
[0162] Injection volume: 25 .mu.L (25 .mu.g per injection)
[0163] UV Wavelength 214 nm, 280 nm
[0164] Mobile phase A: 20 mM sodium phosphate buffer pH 7.5
[0165] Mobile phase B: 25 mM NaCl; 20 mM sodium phosphate buffer pH 7.5
TABLE-US-00004 Time Solvent composition Solvent composition [min] [%-B] [mM NaCl] 0 15.0 3.75 10 15.0 3.75 60 100.0 25.0 62 100.0 25.0 63 15.0 3.75 70 15.0 3.75
[0166] Gradient:
[0167] Table 3 shows the area of the CEX main peak corresponding to antibody molecules without a C-terminal lysine residue (K0):
TABLE-US-00005 parental clone subclone area main K0 (%) CHO cl485-11 8 68.6 cl563-7 54 69.6 cl563-24 103 63.0 reference product -/- -/- 36.0 (mean of 12 samples)
[0168] It is apparent from the above Table 3 that the ustekinumab produced by the method of the present invention has a considerably higher percentage of antibody molecules lacking both C-terminal lysines (referred to as K0) than the reference product.
[0169] 4. Functional characterisation of the ustekinumab antibody 4.1 IL23 ELISA
[0170] Nunc MaxiSorpx.RTM. plates were coated with 50 .mu.l of coating solution (0.5 .mu.g/ml recombinant human IL-23 in PBS). After discarding the coating solution, the plates were washed three times with 350 .mu.l washing buffer (0.1% polysorbate 20 in PBS) per well, before blocking the plates with 1% BSA in PBS and washing one time with the above washing buffer. After discarding the washing buffer, 50 .mu.l of serially diluted antibody preparations were added to each well and the plates were incubated for two hours at room temperature. The plates were then washed three times with 350 .mu.l washing buffer per well and 100 .mu.l of horseradish peroxidase (HRP)-conjugated detection antibody (mouse anti-human IgG HRP conjugate) in 1% BSA/PBS were added to each well. The plates were incubated for 30 minutes at room temperature and then washed three times with 350 .mu.l washing buffer per well. Then 100 .mu.l of the HRP substrate 3,3',5,5'-tetramethylbenzidine (100 .mu.g/ml in DMSO and citrate phosphate buffer, pH 5.0) was added and the plates were incubated. After 10 minutes it was started to measure the absorption at 650 nm and the reaction was stopped when the wells with the highest concentration of standard reached an absorbance value of 1 by adding 50 .mu.l of 2 M sulphuric acid per well. Then the absorption was measured at 450 nm within 30 minutes. The calculation of the relative potency of the test samples was done with the PLA2.1 software.
Table 4 shows the results of the IL23 ELISA test:
TABLE-US-00006 parental clone subclone relative potency [U/mg] CHO cl485-11 8 1.02 cl563-7 54 1.02 cl563-24 103 0.95 reference -/- -/- 1.00 product
[0171] Table 4 shows that despite the differences in sialylation and the different distribution of the glycoforms the ustekinumab antibody produced in CHO cells shows essentially the same binding to its target IL-23 as the reference product.
[0172] 4.2 IL-12 binding
[0173] The binding affinity of ustekinumab biosimilar to IL-12 was analyzed using Biolayer Interferometry (BLI) with an Octet RED96 system (ForteBio). Ustekinumab was immobilized at 0.5 .mu.g/mL using anti-Human IgG Fc Capture (AHC) biosensors and recombinant human IL-12 was allowed to bind in 3 concentrations (0.2, 0.1 and 0.05 .mu.g/mL) for 600 seconds and to dissociate for 2400 seconds. Measurements were done in PBS containing 0.1% BSA and 0.02% Tween20, pH 7.2 at 30.degree. C. The data were evaluated with the Data Analysis 9.0 Software using a 1:1 binding model.
[0174] Table 5 shows the results of the IL-12 binding test:
TABLE-US-00007 parental BLI-IL-12 clone subclone K.sub.D [M] k.sub.on k.sub.off CHO cl563-7 54 2.08E-10 4.75E+05 9.73E-05 cl563-24 103 1.90E-10 5.14E+05 9.72E-05 reference -/- -/- 2.06E-10 4.43E+05 8.94E-05 product
[0175] Similar to the results for IL-23 binding, Table 5 shows that despite the differences in sialylation and the different distribution of the glycoforms the ustekinumab antibody produced in CHO cells shows essentially the same binding to its target IL-12 as the reference product.
[0176] 4.3 FcRn Binding
[0177] The binding of the ustekinumab biosimilar to FcRn was measured using bio-layer interferometry (BLI). Both the FcRn ligand and the antibody samples were diluted in a 96-well plate according to a predetermined scheme using kinetic buffer (0.01% BSA, 0.02% polysorbate 20 in DPBS). Binding of ustekinumab to FcRn was analyzed at pH 6.0 and 30.degree. C. in kinetic buffer using an Octet RED96 System (Pall--ForteBio). The data were evaluated with the Data Analysis 9.0 Software using a 1:1 binding model.
[0178] Table 6 shows the results of the FcRn binding test:
TABLE-US-00008 parental BLI-FcRn clone subclone KD [M] kon koff CHO cl485-11 8 8.96E-10 8.78E+05 7.79E-04 cl563-7 54 9.16E-10 8.50E+05 7.78E-04 cl563-24 103 9.18E-10 8.78E+05 8.08E-04 reference -/- -/- 8.84E-10 8.39E+05 7.40E-04 product
[0179] It is apparent from Table 6 that the ustekinumab antibody produced in CHO cells shows essentially the same binding to FcRn as the reference product.
[0180] 4.3 IFN.gamma. Release
[0181] The relative biological activity of the reference product and the ustekinumab biosimilar was measured by its inhibition of IL-12 induced IFN-.gamma. production in a human natural killer lymphoma cell line (NK-92).
[0182] Stimulation of NK-92 cells with IL-12 induces expression of IFN-.gamma. which is secreted from the cells into the medium supernatant. Ustekinumab which binds and neutralizes the p40 subunit of IL-12 inhibits binding of IL-12 to its cell surface receptors IL12R.delta.1 and IL12R.beta.2, which subsequently results in inhibition of IFN.gamma.-expression. The IFN-.gamma. concentration in the medium is detected with a sandwich enzyme linked immunosorbance assay (ELISA).
[0183] The relative potency is determined by comparison of the inhibitory effect of the test sample to a reference substance.
[0184] NK-92 cells were cultured in suspension at 37.degree. C. in .alpha.-MEM containing 12.5% FCS, 12.5% horse serum and 1% glutamine. IL-2 was added to the medium in a final concentration of 20 ng/ml. Before the assay for IFN.gamma. secretion was started, the cells were IL-2-starved overnight. Serial dilutions of the reference substance and the test samples were prepared. Before treatment of the NK-92 cells the antibody samples were pre-incubated with IL-12 for one hour to allow binding of the antibody to IL-12. 5.times.10.sup.4 NK-92 cells per ml culture medium were seeded in one well of a 96-well plate in IL2-containing medium and then treated with 100 .mu.l of the pre-incubated samples. The cells were incubated for 24 hours at 37.degree. C. and then the supernatants were harvested.
[0185] To determine the IFN-gamma concentration in the supernatants, the Duo Set IFN-gamma ELISA Kit in combination with the Duo Set Ancillary Reagent Kit 2 of R&D Systems were used according to the manufacturer's instructions. The relative potency (RP) was calculated using the PLA2.1 software.
[0186] Table 7 shows the results of the IFN.gamma. release test:
TABLE-US-00009 parental NK-Assay clone subclone RP [U/mg] CHO cl485-11 8 1.10 cl563-7 54 1.09 cl563-24 103 0.98 reference -/- -/- 1.00 product
[0187] It is apparent from Table 7 that the ustekinumab antibody produced in CHO cells inhibits IFN.gamma. release from NK-92 cells to substantially the same degree as the reference product.
[0188] 5. Additional Analysis of Clone Number c1563-24, Subclone 103
[0189] Clone number c1563-24, subclone 103, transfected as described in FIG. 1 was cultured in commercially available media in the fed batch mode. After 15 days of culture the cell supernatant was removed and purified by protein A chromatography. The resulting antibody preparation was subjected to glycoform characterisation using HILIC-UPLC as described in example 2 for the distinction between NANA and NGNA. The results of this analysis are shown in Table 8 below.
TABLE-US-00010 TABLE 8 Relative quantity in Relative quantity in N-Glycan structure biosimilar product (%) reference product (%) Total afucosylation 3.2 6.0 Total high mannose 0.8 0.9 Total sialylation 1.3 20.3* Total galactosylation 36.4 47.3 *includes .alpha.-Gal
[0190] Additionally, the results of the activity assays are shown in Tables 9 to 11 below:
TABLE-US-00011 TABLE 9 FcRn binding - d15 K.sub.D 9.01E-10 K.sub.on 8.63E+05 K.sub.off 7.78E-04
TABLE-US-00012 TABLE 10 Relative potency (Cell-based NK92) d15 Relative potency 1.078
TABLE-US-00013 TABLE 11 Relative potency (IL23-ELISA) d15 Relative potency 1.053
Some Embodiments of the Present Invention Relate to
[0191] 1. Composition containing an ustekinumab antibody, wherein the antibody has a sialic acid content of 0 to 5%. [0192] 2. Composition according to item 1, wherein more than 90% of the sialic acid is N-acetylneuraminic acid. [0193] 3. Composition according to item 1 or 2, wherein less than 10% of the sialic acid is N-glycolylneuraminic acid. [0194] 4. Composition according to any one of the preceding items, wherein at least 50% of the ustekinumab molecules within the composition do not comprise a C-terminal lysine. [0195] 5. Method for producing the composition according to any one of the preceding items, comprising culturing CHO cells which are genetically modified to express the ustekinumab antibody in a suitable culture medium. [0196] 6. Method according to item 5, wherein the CHO cells are CHO-K1 cells or cells derived therefrom. [0197] 7. Method according to item 5 or 6, wherein the CHO cells are cultured in fed-batch mode. [0198] 8. Method according to any one of items 5 to 7, further comprising a step of purifying the ustekinumab antibody. [0199] 9. Composition according to any one of items 1 to 4, being a pharmaceutical composition. [0200] 10. Pharmaceutical composition according to item 9, further containing sucrose, L-histidine, L-histidine monohydrochloride monohydrate and polysorbate 80. [0201] 11. Pharmaceutical composition according to item 9 or 10, containing 90 mg/mL ustekinumab, 1 mg/mL L-histidine/L-histidine monohydrochloride monohydrate, 0.04 mg/mL polysorbate 80 and 76 mg/mL sucrose in water for injection. [0202] 12. Pharmaceutical composition according to any one of items 9 to 11 for use in treating plaque psoriasis or psoriatic arthritis.
Sequence CWU 1
1
21449PRTartificialheavy chain of ustekinumab 1Glu Val Gln Leu Val
Gln Ser Gly Ala Glu Val Lys Lys Pro Gly Glu1 5 10 15Ser Leu Lys Ile
Ser Cys Lys Gly Ser Gly Tyr Ser Phe Thr Thr Tyr 20 25 30Trp Leu Gly
Trp Val Arg Gln Met Pro Gly Lys Gly Leu Asp Trp Ile 35 40 45Gly Ile
Met Ser Pro Val Asp Ser Asp Ile Arg Tyr Ser Pro Ser Phe 50 55 60Gln
Gly Gln Val Thr Met Ser Val Asp Lys Ser Ile Thr Thr Ala Tyr65 70 75
80Leu Gln Trp Asn Ser Leu Lys Ala Ser Asp Thr Ala Met Tyr Tyr Cys
85 90 95Ala Arg Arg Arg Pro Gly Gln Gly Tyr Phe Asp Phe Trp Gly Gln
Gly 100 105 110Thr Leu Val Thr Val Ser Ser Ser Ser Thr Lys Gly Pro
Ser Val Phe 115 120 125Pro Leu Ala Pro Ser Ser Lys Ser Thr Ser Gly
Gly Thr Ala Ala Leu 130 135 140Gly Cys Leu Val Lys Asp Tyr Phe Pro
Glu Pro Val Thr Val Ser Trp145 150 155 160Asn Ser Gly Ala Leu Thr
Ser Gly Val His Thr Phe Pro Ala Val Leu 165 170 175Gln Ser Ser Gly
Leu Tyr Ser Leu Ser Ser Val Val Thr Val Pro Ser 180 185 190Ser Ser
Leu Gly Thr Gln Thr Tyr Ile Cys Asn Val Asn His Lys Pro 195 200
205Ser Asn Thr Lys Val Asp Lys Arg Val Glu Pro Lys Ser Cys Asp Lys
210 215 220Thr His Thr Cys Pro Pro Cys Pro Ala Pro Glu Leu Leu Gly
Gly Pro225 230 235 240Ser Val Phe Leu Phe Pro Pro Lys Pro Lys Asp
Thr Leu Met Ile Ser 245 250 255Arg Thr Pro Glu Val Thr Cys Val Val
Val Asp Val Ser His Glu Asp 260 265 270Pro Glu Val Lys Phe Asn Trp
Tyr Val Asp Gly Val Glu Val His Asn 275 280 285Ala Lys Thr Lys Pro
Arg Glu Glu Gln Tyr Asn Ser Thr Tyr Arg Val 290 295 300Val Ser Val
Leu Thr Val Leu His Gln Asp Trp Leu Asn Gly Lys Glu305 310 315
320Tyr Lys Cys Lys Val Ser Asn Lys Ala Leu Pro Ala Pro Ile Glu Lys
325 330 335Thr Ile Ser Lys Ala Lys Gly Gln Pro Arg Glu Pro Gln Val
Tyr Thr 340 345 350Leu Pro Pro Ser Arg Asp Glu Leu Thr Lys Asn Gln
Val Ser Leu Thr 355 360 365Cys Leu Val Lys Gly Phe Tyr Pro Ser Asp
Ile Ala Val Glu Trp Glu 370 375 380Ser Asn Gly Gln Pro Glu Asn Asn
Tyr Lys Thr Thr Pro Pro Val Leu385 390 395 400Asp Ser Asp Gly Ser
Phe Phe Leu Tyr Ser Lys Leu Thr Val Asp Lys 405 410 415Ser Arg Trp
Gln Gln Gly Asn Val Phe Ser Cys Ser Val Met His Glu 420 425 430Ala
Leu His Asn His Tyr Thr Gln Lys Ser Leu Ser Leu Ser Pro Gly 435 440
445Lys2214PRTartificiallight chain of ustekinumab 2Asp Ile Gln Met
Thr Gln Ser Pro Ser Ser Leu Ser Ala Ser Val Gly1 5 10 15Asp Arg Val
Thr Ile Thr Cys Arg Ala Ser Gln Gly Ile Ser Ser Trp 20 25 30Leu Ala
Trp Tyr Gln Gln Lys Pro Glu Lys Ala Pro Lys Ser Leu Ile 35 40 45Tyr
Ala Ala Ser Ser Leu Gln Ser Gly Val Pro Ser Arg Phe Ser Gly 50 55
60Ser Gly Ser Gly Thr Asp Phe Thr Leu Thr Ile Ser Ser Leu Gln Pro65
70 75 80Glu Asp Phe Ala Thr Tyr Tyr Cys Gln Gln Tyr Asn Ile Tyr Pro
Tyr 85 90 95Thr Phe Gly Gln Gly Thr Lys Leu Glu Ile Lys Arg Thr Val
Ala Ala 100 105 110Pro Ser Val Phe Ile Phe Pro Pro Ser Asp Glu Gln
Leu Lys Ser Gly 115 120 125Thr Ala Ser Val Val Cys Leu Leu Asn Asn
Phe Tyr Pro Arg Glu Ala 130 135 140Lys Val Gln Trp Lys Val Asp Asn
Ala Leu Gln Ser Gly Asn Ser Gln145 150 155 160Glu Ser Val Thr Glu
Gln Asp Ser Lys Asp Ser Thr Tyr Ser Leu Ser 165 170 175Ser Thr Leu
Thr Leu Ser Lys Ala Asp Tyr Glu Lys His Lys Val Tyr 180 185 190Ala
Cys Glu Val Thr His Gln Gly Leu Ser Ser Pro Val Thr Lys Ser 195 200
205Phe Asn Arg Gly Glu Cys 210
uspto.report is an independent third-party trademark research tool that is not affiliated, endorsed, or sponsored by the United States Patent and Trademark Office (USPTO) or any other governmental organization. The information provided by uspto.report is based on publicly available data at the time of writing and is intended for informational purposes only.
While we strive to provide accurate and up-to-date information, we do not guarantee the accuracy, completeness, reliability, or suitability of the information displayed on this site. The use of this site is at your own risk. Any reliance you place on such information is therefore strictly at your own risk.
All official trademark data, including owner information, should be verified by visiting the official USPTO website at www.uspto.gov. This site is not intended to replace professional legal advice and should not be used as a substitute for consulting with a legal professional who is knowledgeable about trademark law.