Diagnostic Method And System
Al Ahmad; Mahmoud F. Y. ; et al.
U.S. patent application number 16/396606 was filed with the patent office on 2019-12-19 for diagnostic method and system. The applicant listed for this patent is United Arab Emirates University. Invention is credited to Mahmoud F. Y. Al Ahmad, Mohamed Al Hemairy, Saad Amin.
| Application Number | 20190380661 16/396606 |
| Document ID | / |
| Family ID | 68838923 |
| Filed Date | 2019-12-19 |





View All Diagrams
| United States Patent Application | 20190380661 |
| Kind Code | A1 |
| Al Ahmad; Mahmoud F. Y. ; et al. | December 19, 2019 |
Diagnostic Method And System
Abstract
Self-diagnosis of diseases is highly desired and very popular nowadays. The present application provides system, methodology, and the like for providing real-time detection of a medical condition.
| Inventors: | Al Ahmad; Mahmoud F. Y.; (Al Ain, AE) ; Al Hemairy; Mohamed; (Al Ain, AE) ; Amin; Saad; (Coventry, GB) | ||||||||||
| Applicant: |
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Family ID: | 68838923 | ||||||||||
| Appl. No.: | 16/396606 | ||||||||||
| Filed: | April 26, 2019 |
Related U.S. Patent Documents
| Application Number | Filing Date | Patent Number | ||
|---|---|---|---|---|
| 15383481 | Dec 19, 2016 | |||
| 16396606 | ||||
| 62377223 | Aug 19, 2016 | |||
| Current U.S. Class: | 1/1 |
| Current CPC Class: | A61B 2505/07 20130101; A61B 5/1118 20130101; A61B 5/7246 20130101; A61B 5/087 20130101; A61B 5/01 20130101; A61B 5/747 20130101; A61B 5/0533 20130101; A61B 2562/0219 20130101; A61B 5/14542 20130101; A61B 2562/029 20130101; A61B 5/02416 20130101; A61B 5/746 20130101; A61B 5/02208 20130101; A61B 5/0816 20130101; A61B 5/14532 20130101; A61B 5/0488 20130101; A61B 5/7264 20130101; A61B 5/0402 20130101 |
| International Class: | A61B 5/00 20060101 A61B005/00 |
Claims
1. A system for passively diagnosing a subject, the system comprising: at least one sensor couplable to the subject for collecting at least one measurement from the subject; at least one storage device for storing the collected at least one measurement; and at least one processor in communication with the at least one sensor, the at least one processor configured to: obtain the at least one measurement; determine a weighting factor value to the at least one sensor; determine a control value for the at least one sensor, the control value based on the at least one measurement from the at least one sensor; determine an indicator value based on the at least one measurement, the weighting factor value and the control value; access a database stored on the at least one storage device, the database having at least one predetermined indicator value corresponding to a pre-identified disease; and diagnosing presence of a disease in the subject by solely relying on the at least one measurement and by matching the determined indicator value with the at least one pre-determined indicator value of the pre-identified disease.
2. The system according to claim 1, wherein the at least one measurement is a physiological measurement corresponding to a vital sign of the subject.
3. The system according to claim 1, wherein the control value is a binary value determined as 0 when the at least one measurement is within a known normal range for the at least one pre-determined disease and is determined as 1 when the at least one measurement is outside the normal range for the at least one pre-determined disease.
4. The system according to claim 1, wherein the weighting factor value is the ratio of a number of pre-determined diseases for which the at least one sensor is used to obtain a measurement over a total number of pre-determined diseases in the database.
5. The system according to claim 1, the processor is further configured to determine a minimum value for the at least one pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined minimum range value measurable by the at least one sensor and the control value of the sensor and to determine a maximum value for the pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined maximum range value measurable by the at least one sensor and the control value of the sensor, wherein the minimum value and maximum value are stored in the database.
6. The system according to claim 5, wherein the processor is configured to diagnose the subject as normal if the at least one measurement falls within the pre-determined minimum range value and the predetermined maximum range value for a pre-determined disease.
7. The system according to claim 5, wherein the processor is configured to diagnose the subject as having the pre-determined disease if the indicator value falls within the minimum value and the maximum value for the least one pre-determined disease.
8. The system according to claim 7, the processor is further configured to notify at least one of the subject, a doctor, a hospital, an emergency contact and an emergency mobile unit of the diagnosed disease of the subject.
9. The system according to claim 3, wherein when the at least one sensor is assigned a control value of 0, the processor is configured to eliminate the at least one sensor from further consideration thereby reducing processing time.
10. A method of diagnosing a subject, the method comprising configuring at least one processor to perform the steps of: receiving at least one measurement from at least one sensor non-invasively couplable to the subject; determining a weighting factor value to the at least one sensor; determining a control value for the at least one sensor, the control value based on the at least one measurement from the at least one sensor; determining an indicator value based on the at least one measurement, the weighting factor value and the control value; accessing a database stored on at least one storage device, the database having at least one predetermined indicator value corresponding to a pre-identified disease; and diagnosing presence of a disease in the subject by solely relying on the at least one measurement and by matching the determined indicator value with the at least one pre-determined indicator value of the pre-identified disease.
11. The method according to claim 10, wherein determining the control value comprising assigning a value of 0 when the at least one measurement is within a known normal range for the at least one pre-determined disease and is assigned a value of 1 when the at least one measurement is outside the normal range for the at least one pre-determined disease.
12. The method according to claim 10, wherein determining the weighting factor comprises determining a ratio of a number of pre-determined diseases for which the at least one sensor is used to obtain a measurement over a total number of pre-determined diseases in the database.
13. The method according to claim 10, the method further comprising configuring the at least one processor to further perform the steps of determining a minimum value for the at least one pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined minimum range value measurable by the at least one sensor and the control value of the sensor and determining a maximum value for the pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined maximum range value measurable by the at least one sensor and the control value of the sensor, and storing the determined minimum value and maximum value in the database.
14. The method according claim 13, wherein diagnosing presence of a disease in the subject comprises diagnosing the subject as normal if the at least one measurement falls within the pre-determined minimum range value and the predetermined maximum range value for a pre-determined disease.
15. The method according claim 13, wherein diagnosing presence of a disease in the subject comprises diagnosing the subject as having the pre-determined disease if the indicator value falls within the minimum value and the maximum value for the least one pre-determined disease.
16. The method according to claim 15, the method further comprising notifying at least one of the subject, a doctor, a hospital, an emergency contact and an emergency mobile unit of the diagnosed disease of the subject.
17. The system according to claim 11, wherein by assigning the at least one sensor a control value of 0, configuring the processor to eliminate the at least one sensor from further consideration thereby reducing processing time.
18. The method according to claim 10, the method further comprising: adding a new pre-determined disease to the database; and modifying the weighting factor value based on the added pre-determined disease, thereby enhancing the accuracy of the weighing factor.
19. The system according to claim 1, wherein the disease is at least one of a physical, physiological or emotional disease.
Description
CROSS-REFERENCE TO RELATED APPLICATIONS
[0001] This application is a continuation in part application from U.S. application Ser. No. 15/383,481, filed on Dec. 19, 2016, which claims priority to U.S. Provisional Application No. 62/377,223, filed on Aug. 19, 2016, the entirety of both applications are hereby incorporated by reference.
FIELD OF THE INVENTION
[0002] The present disclosure relates to disease detection and related system and methodology.
BACKGROUND
[0003] Vital signs are commonly used to monitor human's body basic functions. Examples of vital signs that are frequently monitored are body temperature, blood pressure, heart rate, and breathing rate. These indicators help in assessing the physical health of a person by providing diagnosis of possible diseases and checking treatment progress towards recovery. There is a desire in the field for an inexpensive, efficient, accurate and consistent disease diagnostic system and method, that does not rely on the subjectivity of the physician nor the feedback of the patient.
SUMMARY OF THE INVENTION
[0004] The current disclosure describes multiple aspects and embodiments. In one aspect, a system for passively diagnosing a subject is described. An exemplary embodiment of that system comprises: at least one sensor couplable to the subject for collecting at least one measurement from the subject. The system also includes at least one storage device for storing the collected at least one measurement and at least one processor in communication with the at least one sensor. The at least one processor is configured to: obtain the at least one measurement; determine a weighting factor value to the at least one sensor; determine a control value for the at least one sensor, where the control value is based on the at least one measurement from the at least one sensor; determine an indicator value based on the at least one measurement, the weighting factor value and the control value; access a database stored on the at least one storage device, where the database have at least one predetermined indicator value corresponding to a pre-identified disease; and diagnosing presence of a disease in the subject by solely relying on the at least one measurement and by matching the determined indicator value with the at least one pre-determined indicator value of the pre-identified disease.
[0005] In a related embodiment, the at least one measurement is a physiological measurement corresponding to a vital sign of the subject. In another related embodiment, the disease is related to a physical and/or emotional condition of the subject.
[0006] In a related embodiment, the control value is a binary value determined as 0 when the at least one measurement is within a known normal range for the at least one pre-determined disease and is determined as 1 when the at least one measurement is outside the normal range for the at least one pre-determined disease.
[0007] In a related embodiment, the weighting factor value is found as the ratio of a number of pre-determined diseases for which the at least one sensor is used to obtain a measurement over a total number of pre-determined diseases in the database.
[0008] In yet another related embodiment, the processor is further configured to determine a minimum value for the at least one pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined minimum range value measurable by the at least one sensor and the control value of the sensor and to determine a maximum value for the pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined maximum range value measurable by the at least one sensor and the control value of the sensor, wherein the minimum value and maximum value are stored in the database.
[0009] In a further related embodiment, the processor is configured to diagnose the subject as normal if the at least one measurement falls within the pre-determined minimum range value and the predetermined maximum range value for a pre-determined disease. The processor may also be configured to diagnose the subject as having the pre-determined disease if the indicator value falls within the minimum value and the maximum value for the least one pre-determined disease.
[0010] In a related embodiment, the processor is further configured to notify at least one of the subject, a doctor, a hospital, an emergency contact and an emergency mobile unit of the diagnosed disease of the subject.
[0011] In one related embodiment, when the at least one sensor is assigned a control value of 0, the processor is configured to eliminate the at least one sensor from further consideration thereby reducing processing time.
[0012] Another aspect of the invention may be described as a method of diagnosing a subject, the method comprising configuring at least one processor to perform the steps of: receiving at least one measurement from at least one sensor non-invasively couplable to the subject; determining a weighting factor value to the at least one sensor; determining a control value for the at least one sensor, the control value based on the at least one measurement from the at least one sensor; determining an indicator value based on the at least one measurement, the weighting factor value and the control value; accessing a database stored on at least one storage device, where the database having at least one predetermined indicator value corresponding to a pre-identified disease; and diagnosing presence of a disease in the subject by solely relying on the at least one measurement and by matching the determined indicator value with the at least one pre-determined indicator value of the pre-identified disease.
[0013] In a related embodiment, the step of determining the control value comprises assigning a value of 0 when the at least one measurement is within a known normal range for the at least one pre-determined disease and is assigned a value of 1 when the at least one measurement is outside the normal range for the at least one pre-determined disease.
[0014] In another related embodiment, the step of determining the weighting factor comprises determining a ratio of a number of pre-determined diseases for which the at least one sensor is used to obtain a measurement over a total number of pre-determined diseases in the database.
[0015] In yet another embodiment, the method further comprises configuring the at least one processor to further perform the steps of determining a minimum value for the at least one pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined minimum range value measurable by the at least one sensor and the control value of the sensor and determining a maximum value for the pre-determined indicator based on the weighting factor value of the at least one sensor, a pre-determined maximum range value measurable by the at least one sensor and the control value of the sensor, and storing the determined minimum value and maximum value in the database.
[0016] In a related embodiment, the step of diagnosing presence of a disease in the subject comprises diagnosing the subject as normal if the at least one measurement falls within the pre-determined minimum range value and the predetermined maximum range value for a pre-determined disease.
[0017] In a related embodiment, the step of diagnosing presence of a disease in the subject comprises diagnosing the subject as having the pre-determined disease if the indicator value falls within the minimum value and the maximum value for the least one pre-determined disease.
[0018] In another related embodiment, the method further comprising notifying at least one of the subject, a doctor, a hospital, an emergency contact and an emergency mobile unit of the diagnosed disease of the subject.
[0019] In a further related embodiment, by assigning the at least one sensor a control value of 0, the method include configuring the processor to eliminate the at least one sensor from further consideration thereby reducing processing time.
[0020] In another related embodiment, the method further comprises adding a new pre-determined disease to the database; and modifying the weighting factor value based on the added pre-determined disease, thereby enhancing the accuracy of the weighing factor.
BRIEF DESCRIPTION OF THE DRAWINGS
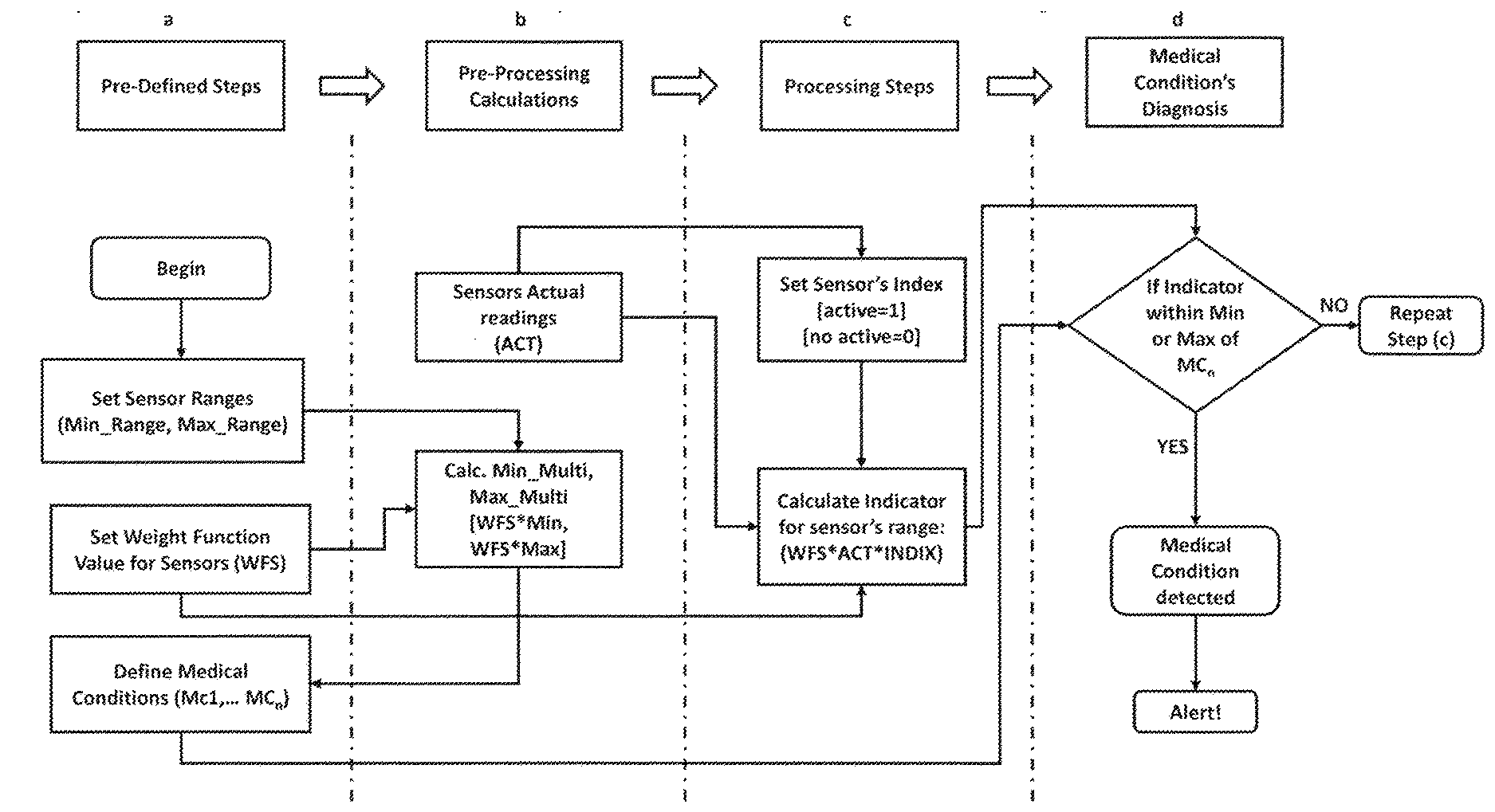
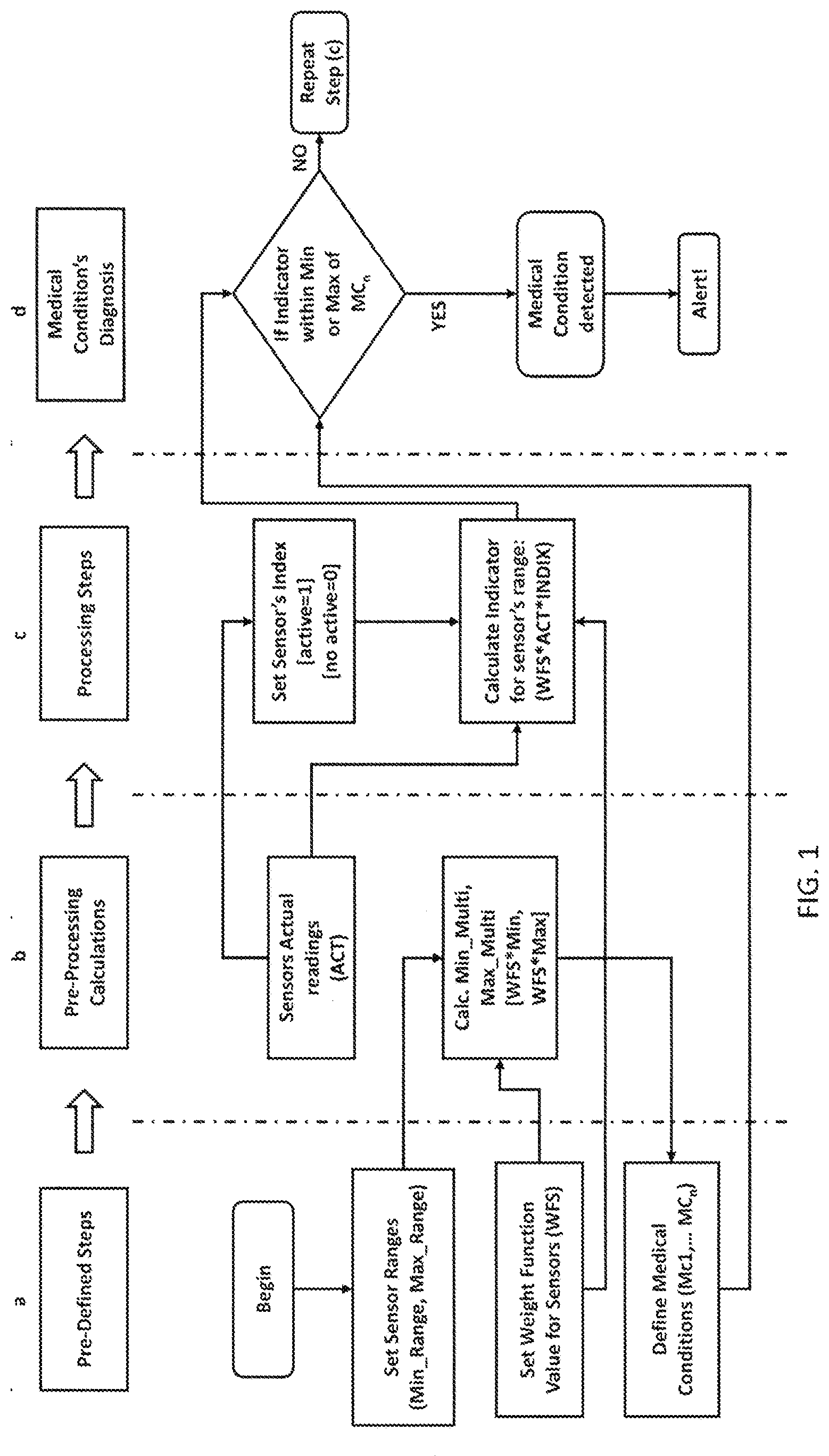
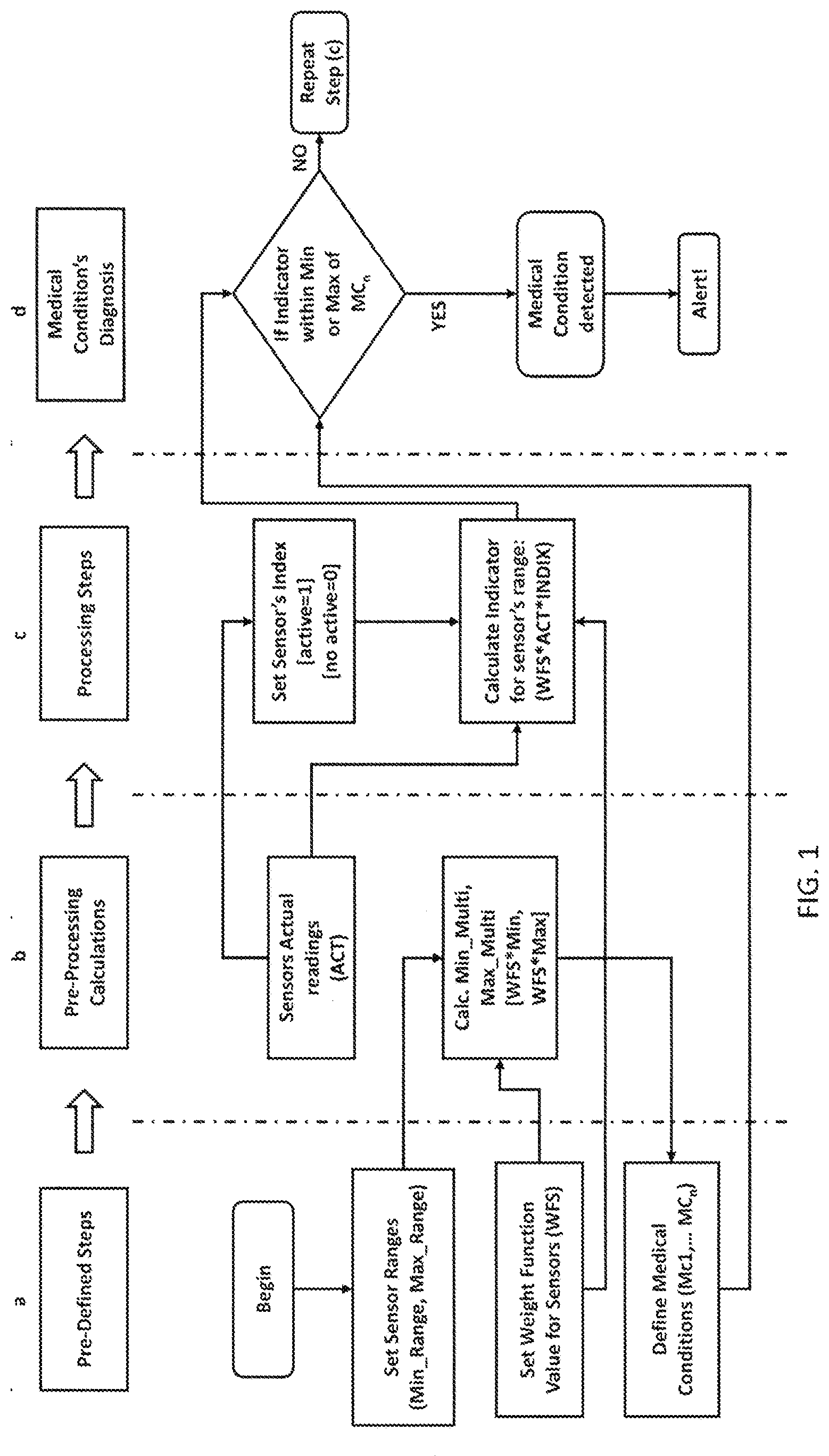
[0021] FIG. 1: shows a workflow diagram illustrating an online system architecture according to an embodiment of the current invention. The workflow has four stages: a, b, c, and d.
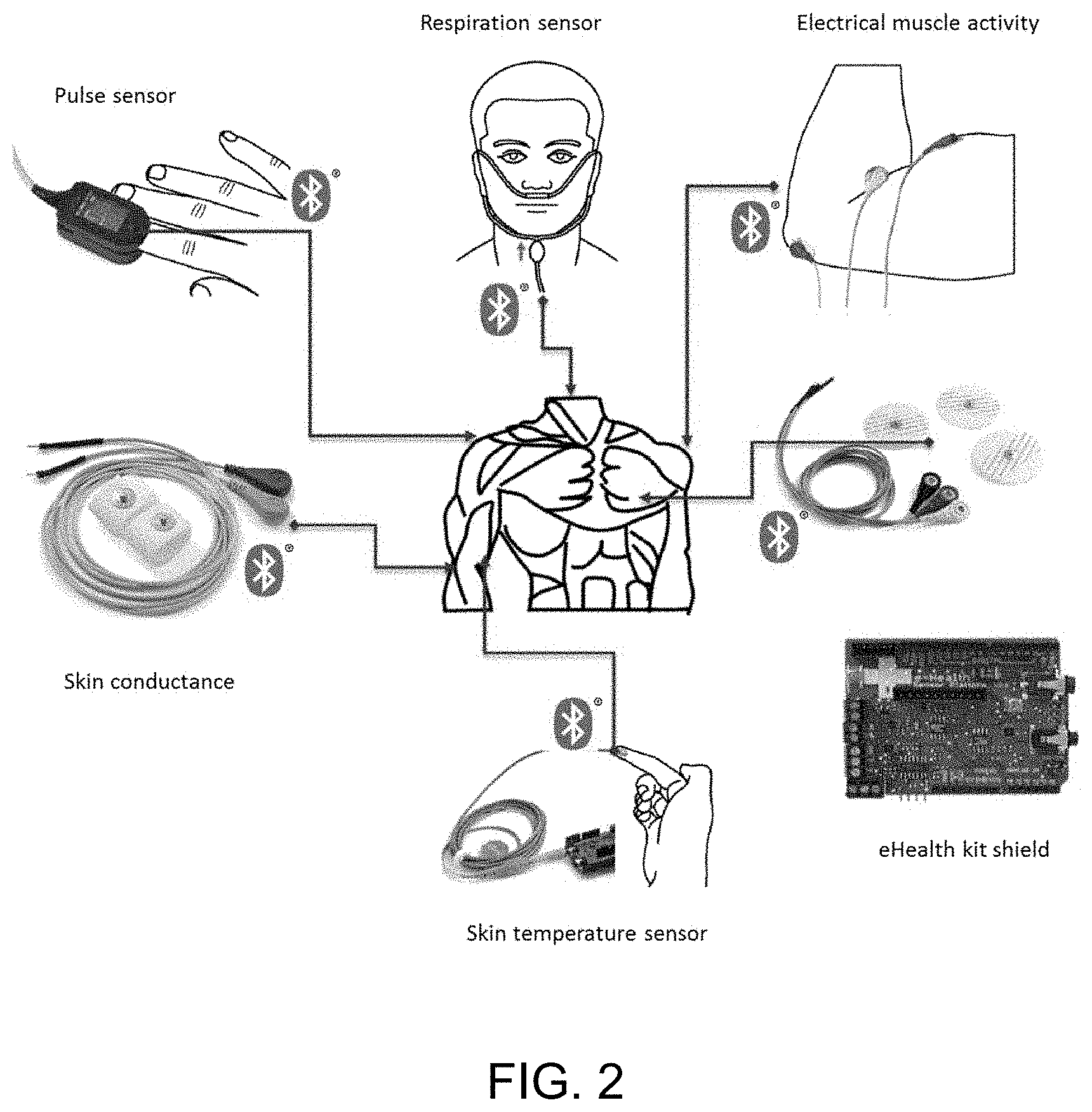
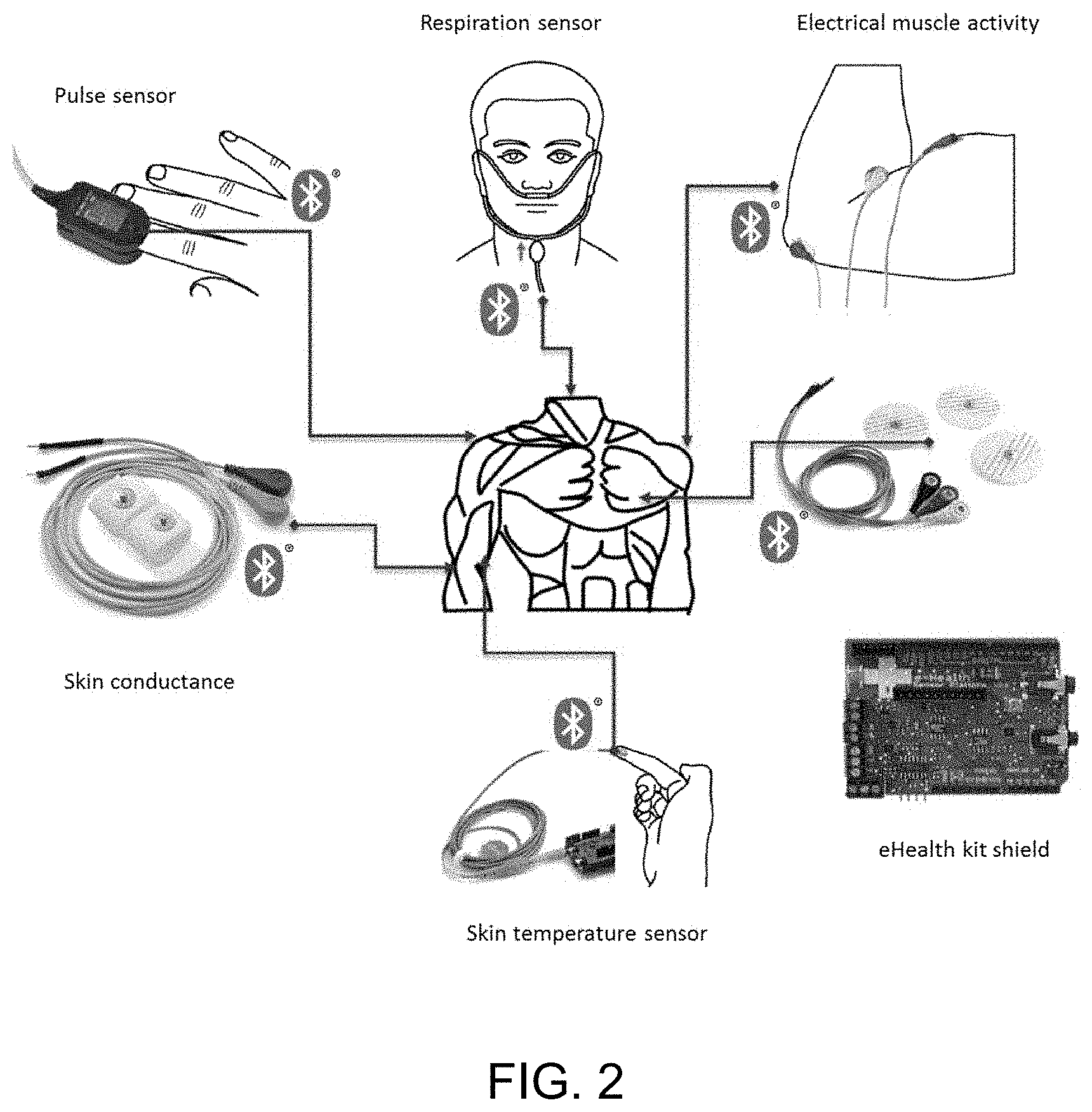
[0022] FIG. 2: shows a platform for measuring biometrics according to an exemplary embodiment of the invention.
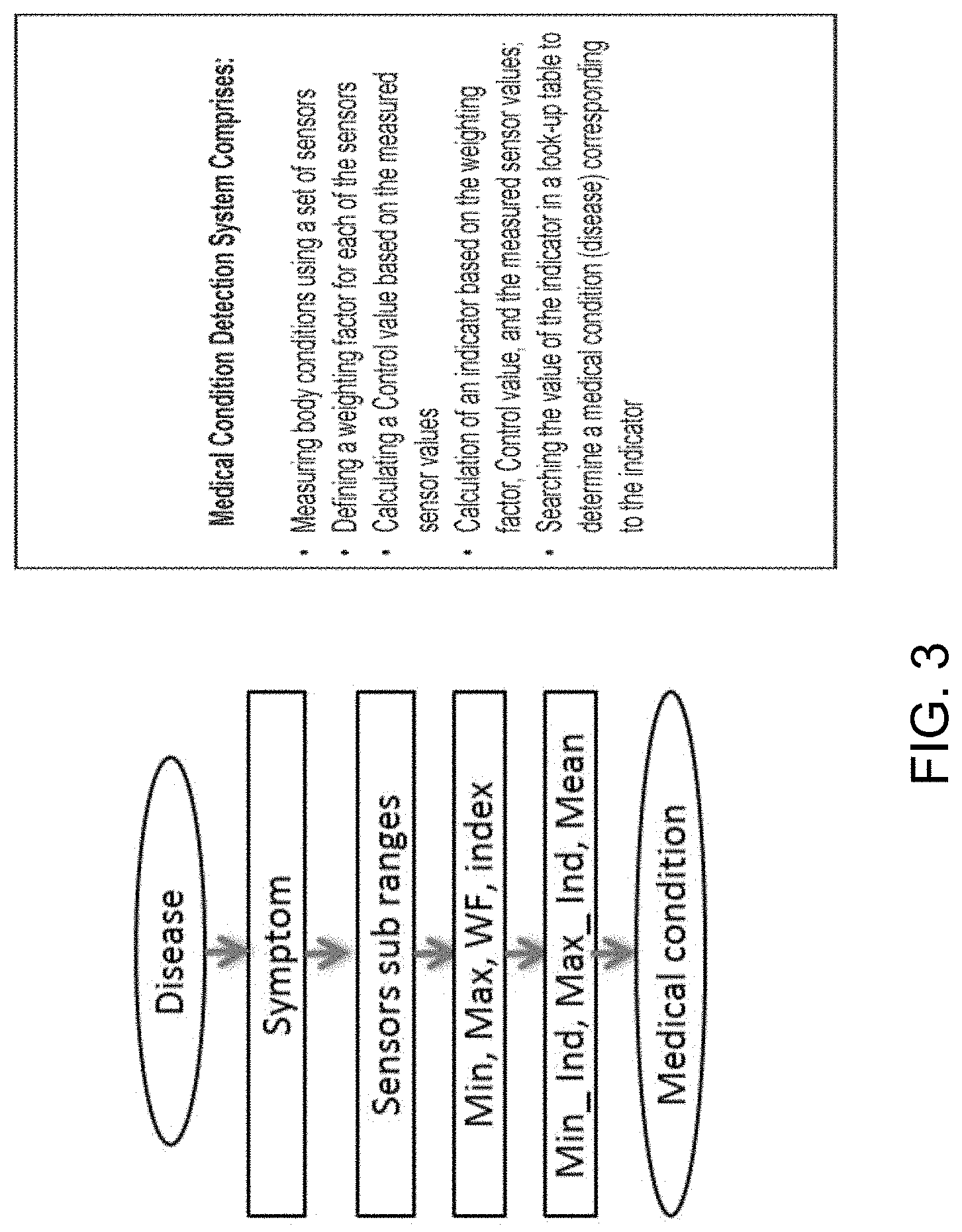
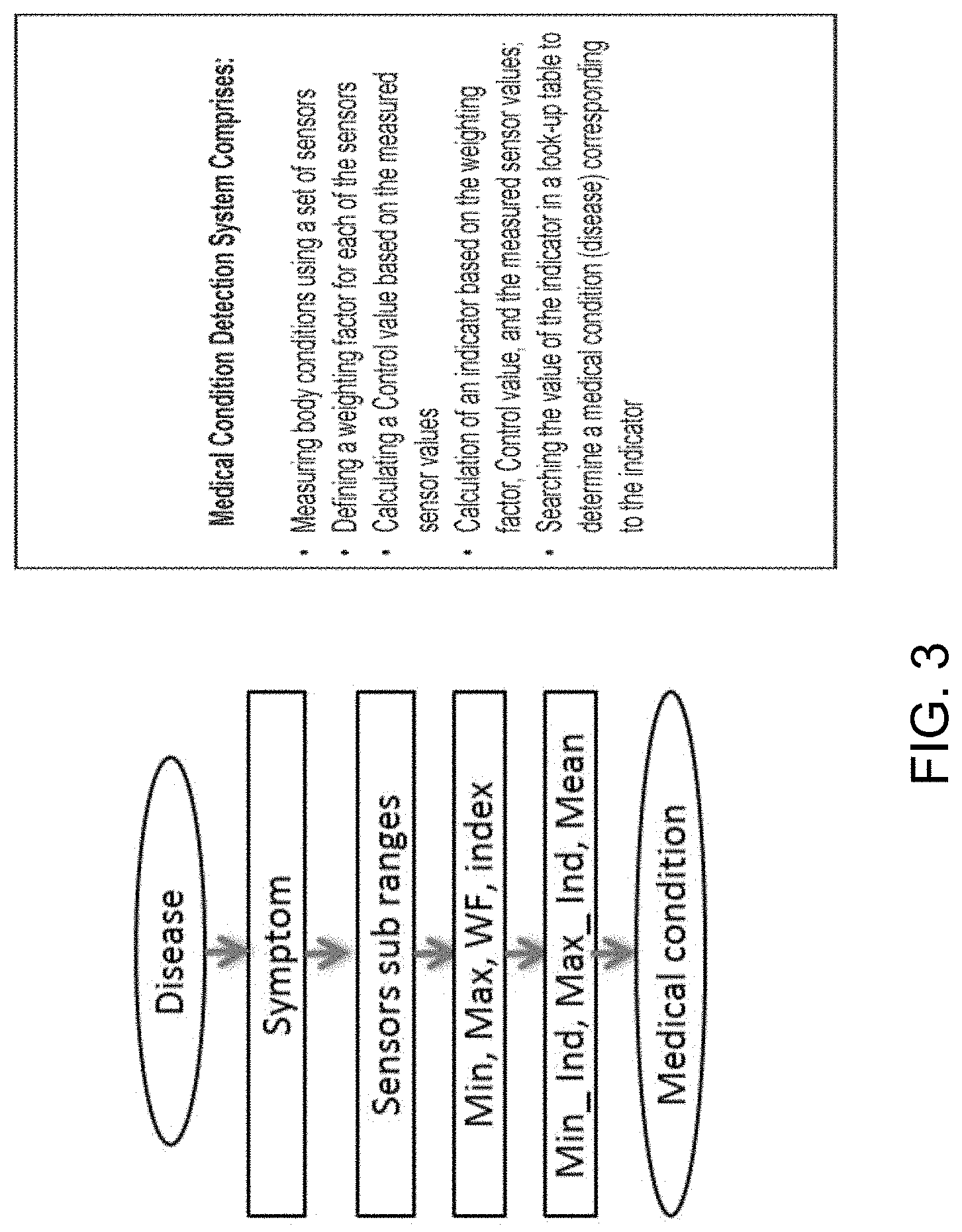
[0023] FIG. 3: shows a medical condition detection system according to an exemplary embodiment of the invention.
[0024] FIG. 4: shows an exemplary disease diagnosis system.
[0025] FIG. 5: shows a pseudocode for Disease Search Algorithm according to an embodiment of the invention.
[0026] FIG. 6: shows an exemplary eHealth test bench system.
[0027] FIG. 7: shows a wearable sensor simulator system according to an exemplary embodiment of the invention.
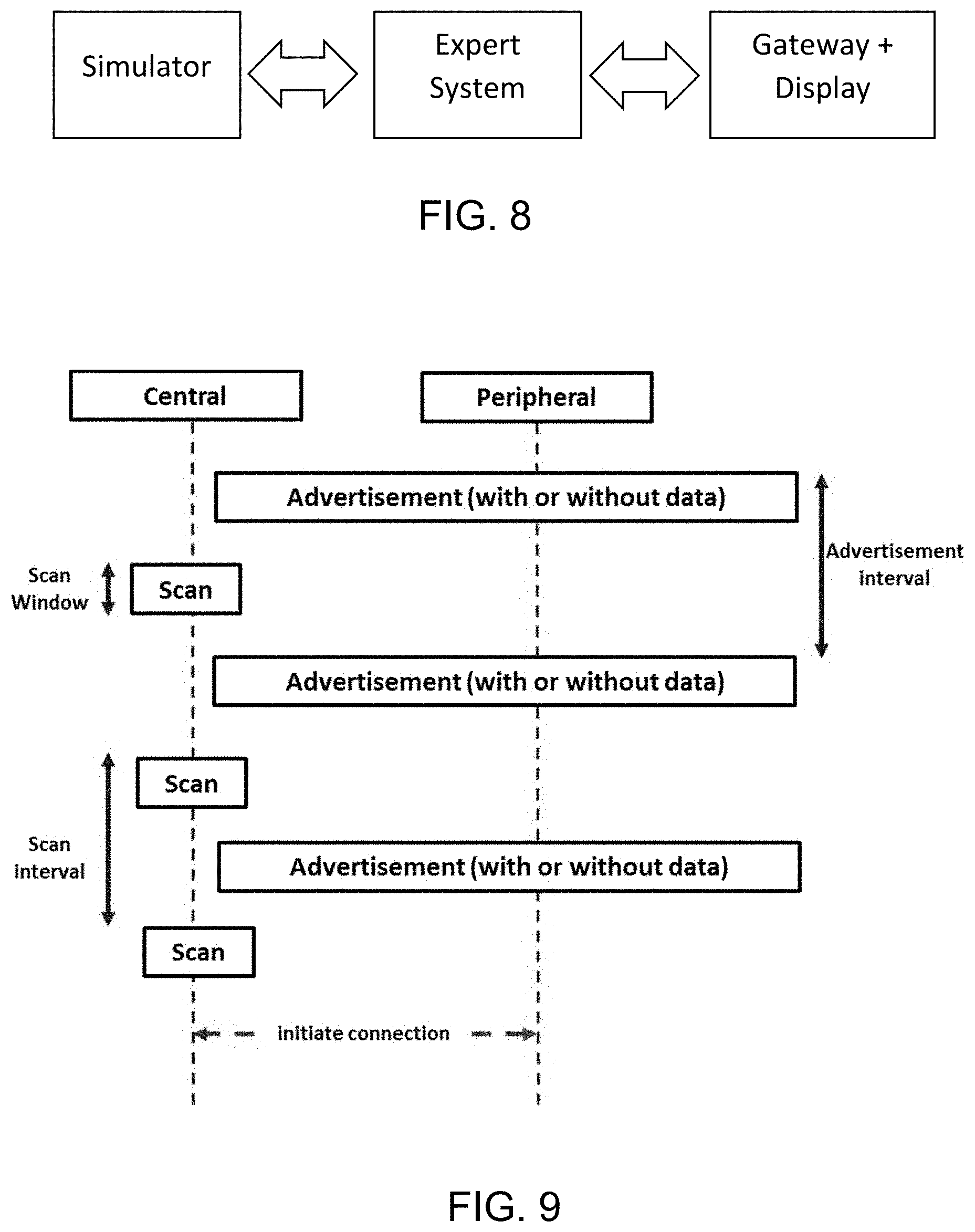
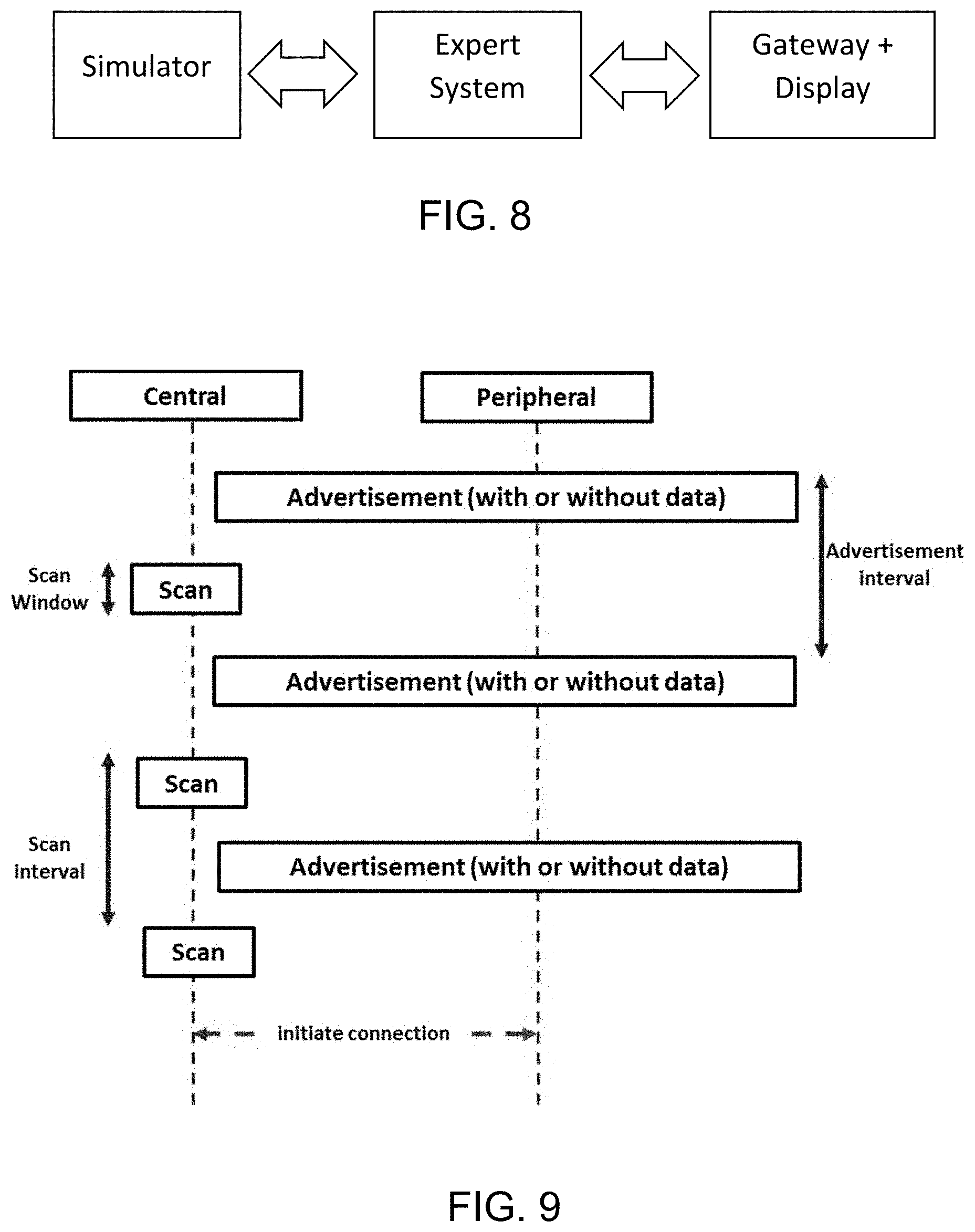
[0028] FIG. 8: shows an evaluation system according to an embodiment of the invention, the system comprising a simulator, gateway, display, and a server.
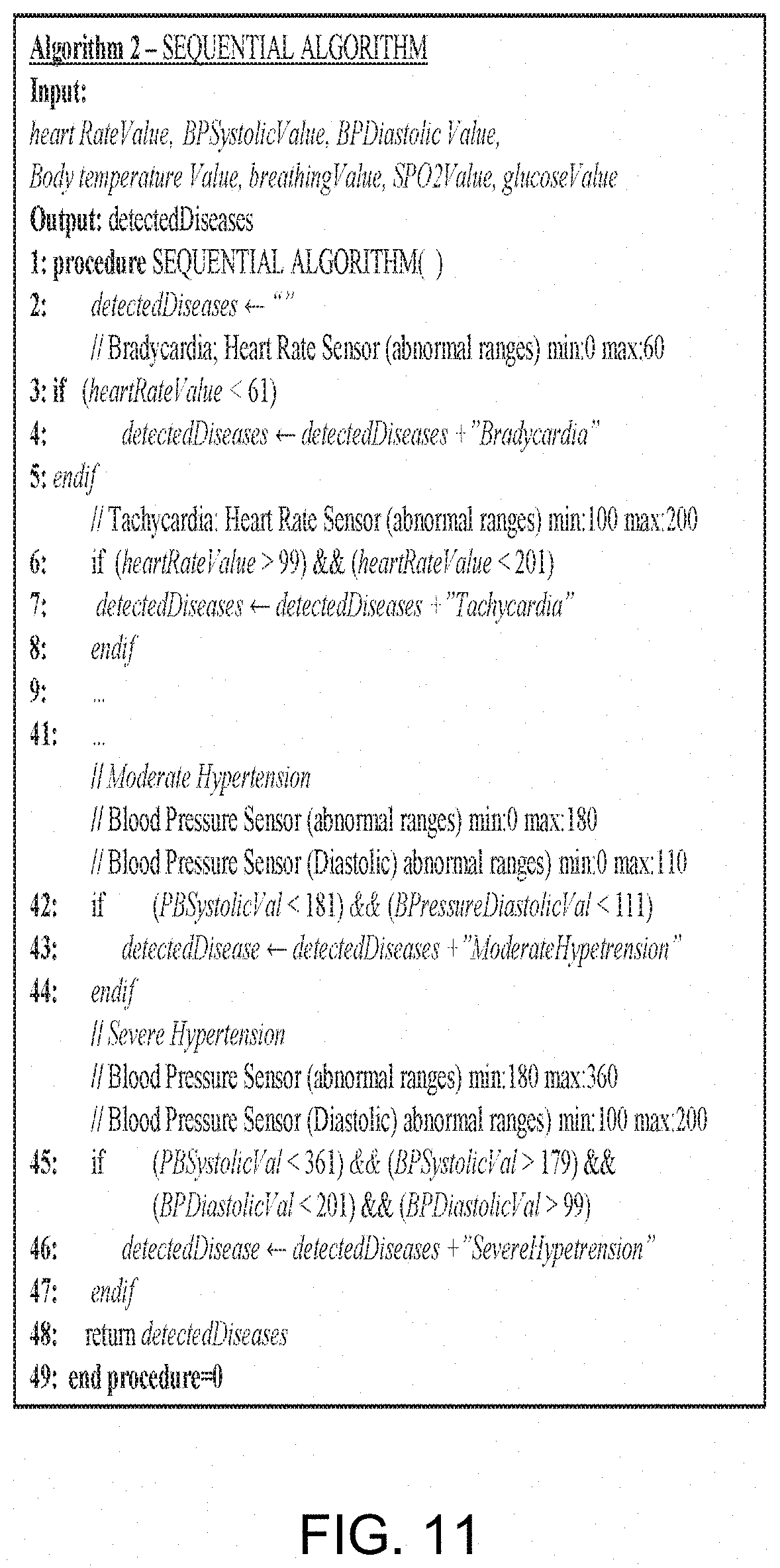
[0029] FIG. 9: shows a flowchart of data transfer from sensors simulator (Peripheral) to medical gateway (Central).
[0030] FIG. 10: shows transfer time from medical gateway to server over several tests.
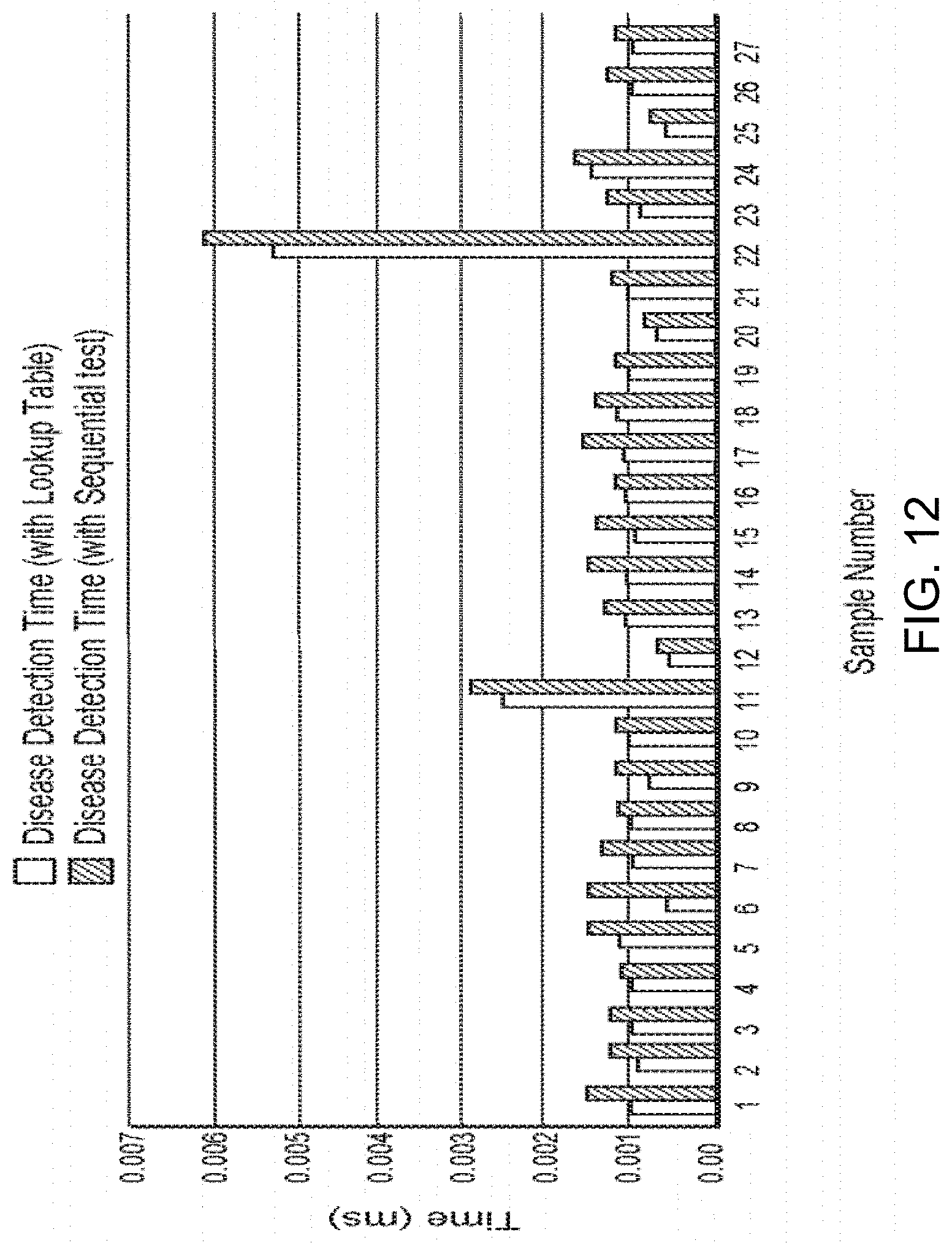
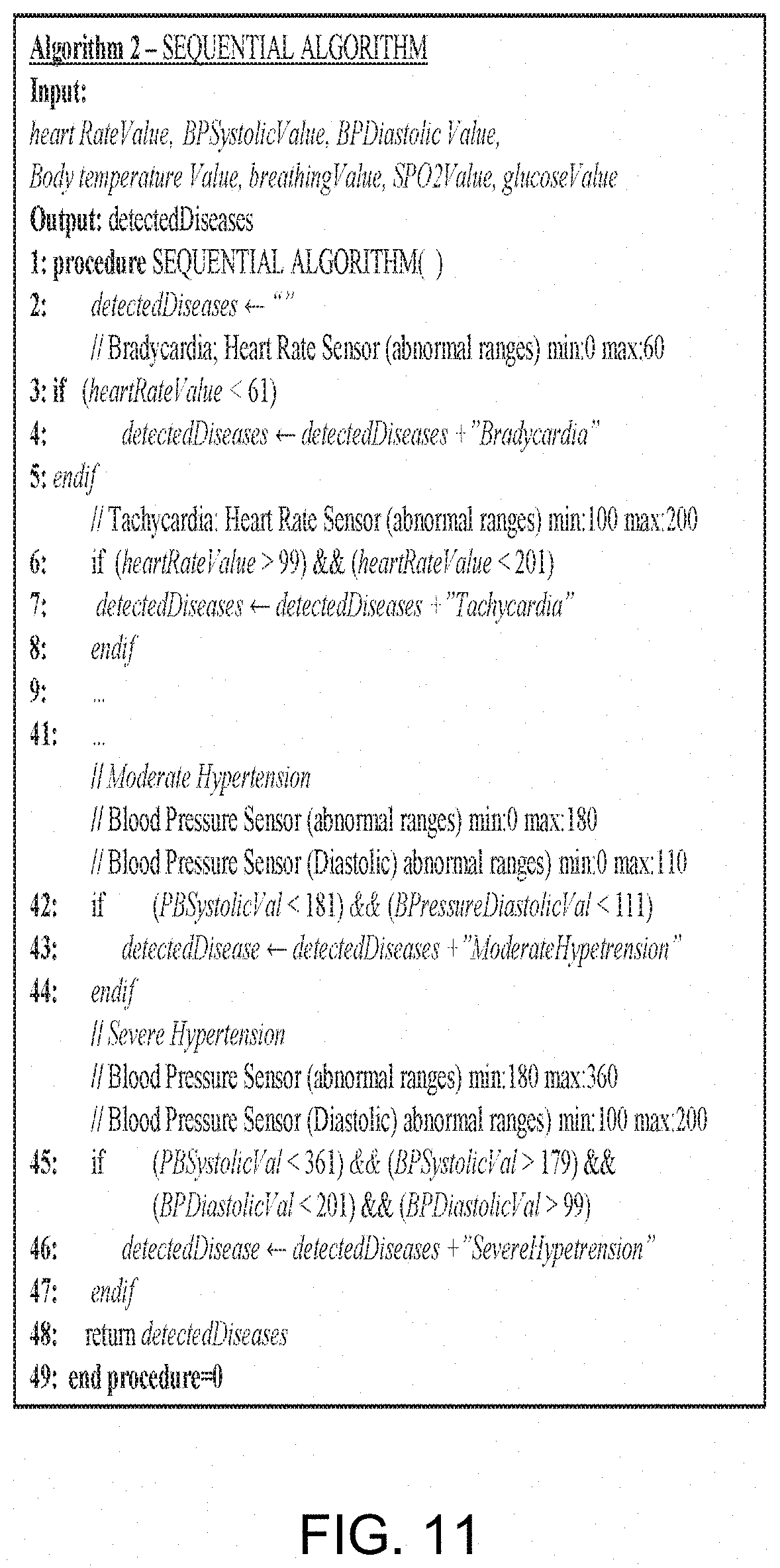
[0031] FIG. 11: shows pseudocode for a Sequential Search Algorithm that is used in the prior art.
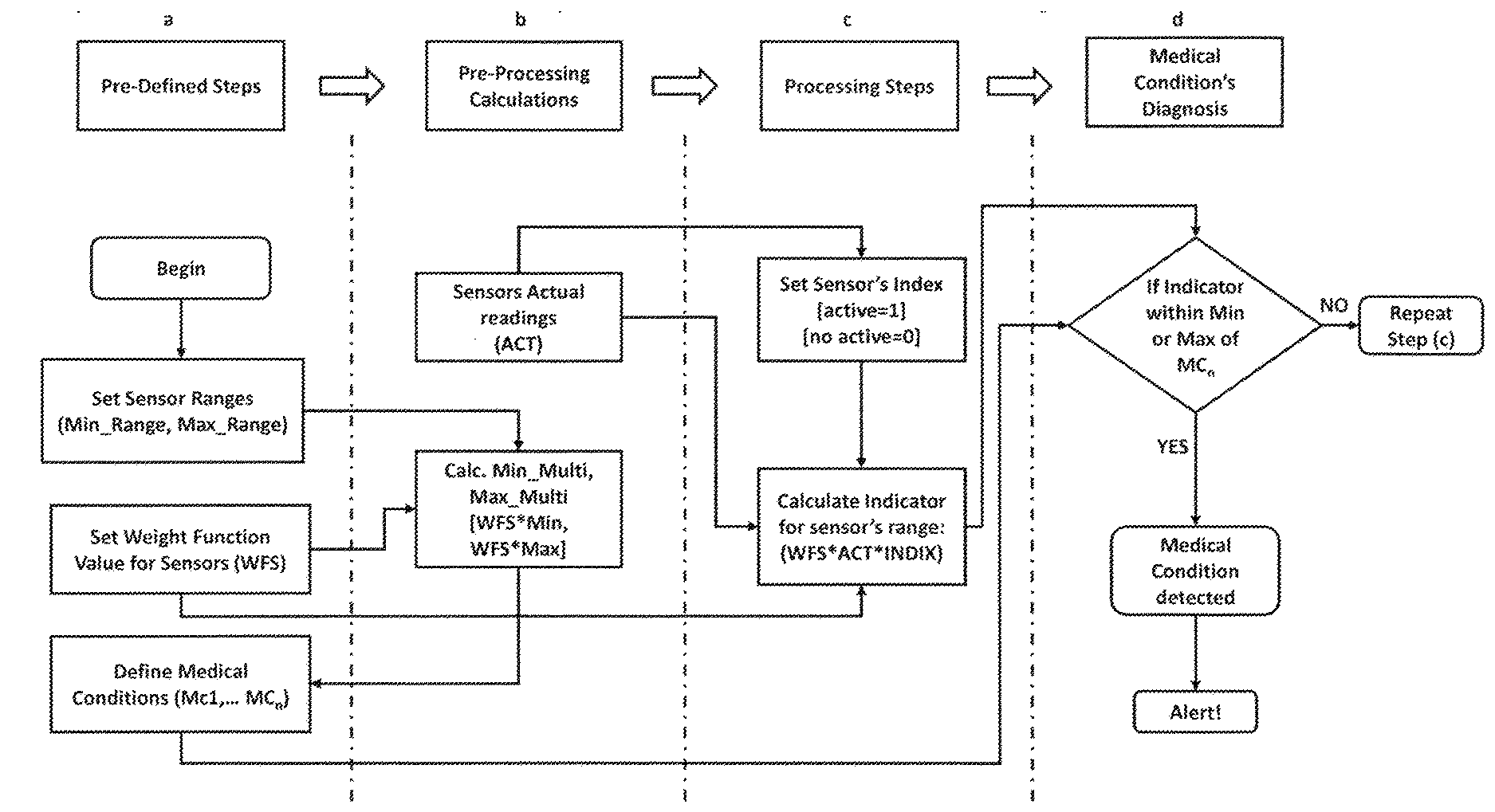
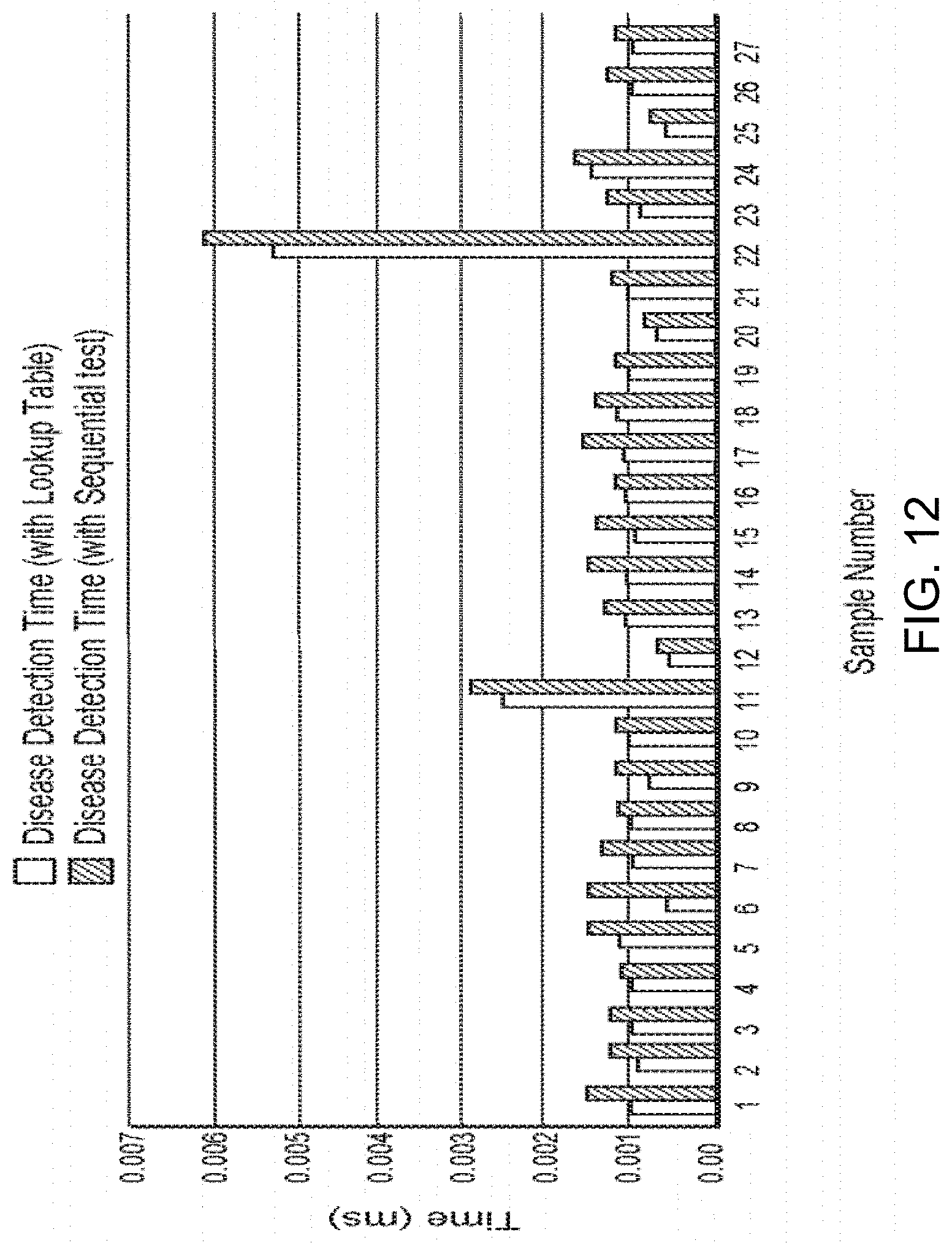
[0032] FIG. 12: shows a comparison chart of disease detection time using the exemplary eHealth system and lookup table.
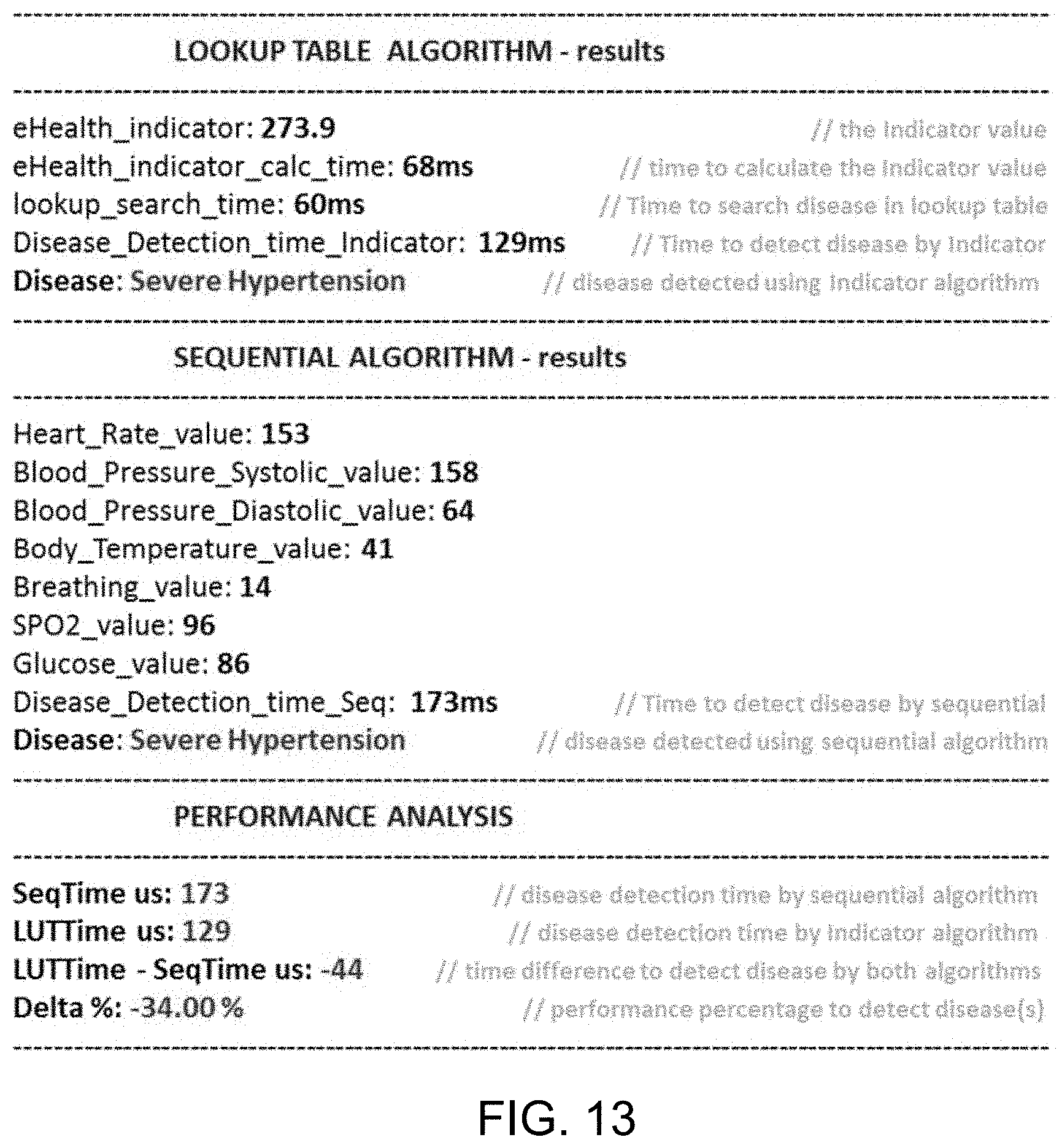
[0033] FIG. 13: Real-time testing on server for performance in detecting diseases.
DETAILED DESCRIPTION
[0034] Vital signs such as body temperature, blood pressure, heart rate, and breathing rate, by way of nonlimiting examples, are commonly used to monitor human's body basic functions, These indicators help in assessing the physical health of a person by providing diagnosis of possible diseases, and checking treatment progress towards recovery. Table 1 shows some common diseases along with their corresponding medical conditions and sensors used to measure associated vital sign alteration. Table 1 also provides a brief description of each disease.
TABLE-US-00001 TABLE 1 Defined diseases and corresponding medical conditions Disease Description Vital signs ranges Associated sensor/s Bradycardia abnormally slow heart rate <60 beats/min HR_SENSOR Tachycardia abnormally fast heart rate >100 OR > 120 beats/min HR_SENSOR Hypotension abnormally low blood pressure BP < 100 mm Hg systolic BP_SENSOR Hypertension abnormally high blood pressure Mild to moderate (systolic BP_SENSOR blood pressure < 180 mm Hg and diastolic blood pressure below 110 mm Hg) Severe hypertension, BP_SENSOR defined as a systolic pressure > 180 mm Hg or diastolic pressure > 110 mm Hg, Hypoxaemia abnormally low concentration of oxygen SP02 < 95% SP02_SENSOR in the blood Hyperthermia abnormally high body temperature core temperature > 37.80.degree. C. TEMP_SENSOR Hypothermia Abnormally low body temperature core temperature < 36.0.degree. C. TEMP_SENSOR Bradypnea abnormally slow breathing rate RR < 20 breaths/min RR_SENSOR Tachypnea abnormally fast breathing rate RR > 25 breaths/min RR_SENSOR Sinus P waves are hidden within each preceding ECG image "camel hump" ECG_SENSOR Tachycardia T wave appearance Prediabetes blood sugar level is higher than normal Fasting glucose level: GLOCOSE_SENSOR but not yet high enough to be classified as (100-125) (mg/dL) type 2 diabetes Diabetes describes a group of metabolic diseases in Fasting glucose level: GLOCOSE_SENSOR which the person has high blood glucose more than 125 (mg/dL) (blood sugar), either because insulin production is inadequate, or because the body's cells do not respond properly to insulin, or both Pneumonia a disease of the lungs characterized RR > 25 breaths/min RR_SENSOR especially by inflammation and HR > 100 OR HR > 120 beats/min HR_SENSOR consolidation of lung tissue followed by core temperature > 37.80.degree. C. TEMP_SENSOR resolution and by fever, chills, cough, and difficulty in breathing and that is caused especially by infection Urosepsis is a systemic reaction of the body (SIRS) core temperature > 37.80.degree. C. TEMP_SENSOR to a bacterial infection of the urogenital HR > 100 or HR > 120 beats/min HR_SENSOR organs with the risk of life-threatening BP < 100 mm Hg systolic BP_SENSOR symptoms including shock Asthma is a chronic inflammatory disorder of the 90% < SPO2 < 95% SP02_SENSOR Moderate airways 100 < HR < 120 beats/min HR_SENSOR RR > 25 breaths/min RR_SENSOR Asthma is sever chronic inflammatory disorder of SP02 < 90% SP02_SENSOR Severe the airways HR > 120 beats/min HR_SENSOR RR > 25 breaths/min RR_SENSOR Respiratory is the cessation of normal breathing due SP02 < 90% SP02_SENSOR Arrest to failure of the lungs to function effectively HR < 60 beats/min HR_SENSOR Imminent RR > 30 breaths/min RR_SENSOR
[0035] Detection and identification of diseases at early stage can facilitate and possibly improve success of the treatment significantly. Unfortunately, due to the load of the daily work, most people do not find enough time to visit the doctor. On the other hand, due to the frequent increment of diseases nowadays, it becomes impossible for the physicians to recall all symptoms and medical conditions for all kind of diseases. Adequate assistive tools are necessary not only to help quickly identify the diseases but also to minimize medical mistakes and avoid prescribing inaccurate or unnecessary medications or treatments. Online diagnosis system may be used to provide such diagnosis services. IN such systems, the accurate detection and identification of a disease is highly dependable on the method used for diagnosis.
[0036] However, disease diagnosis is a very sophisticated process and demands high and advance level of expertise and it is an expensive and taxing process in terms of computational time and energy consumption. A highly selective and efficient web-based clinical expert system is not yet developed in spite of the ongoing and existing trails and available systems. Existing expert system incorporates inference rules. Those rules play significant role in suggesting specific methods for disease diagnosis and treatment. Currently, there are several reports on e-health management systems that employ different diagnostic tools. There is are ongoing scientific discussions and debate about which kind of diseases should be included in medical diagnosis expert system along with their symptoms, which factors should be considered in diagnosis for such system and what approach should be followed, etc.
[0037] The current disclosure provides system, methodology, and the like for diagnosing any kind of disease. In one embodiment, the current disclosure provides a system comprising one or more computing devices configured to perform operations consistent with an algorithm order to determine a variable called an "indicator" (also referred to as "eHealth Indicator") and its minimum and maximum interval values. The system then uses this "Indicator" value to search a look up table for the predefined corresponding disease, which may be stored on a storage device in communication with the processor. The storage device may be integral to the processing system or may be independent of it. The instant system is experimented on various scenarios and a software simulator has been developed for evaluation and performance testing.
[0038] As detailed below, the present inventors developed a systematic procedure for self-diagnosis of diseases, using a support system developed and tested. In the examples provided, the system may perform operations that detect potential occurrences of, and compute indicia of, several medical conditions. Each medical condition is associated with specific symptoms and signs that are mapped directly with several kinds of sensors and their readings. It is to be understood that the types of medical conditions presented in this disclosure as well as their indicia are only exemplary and are not intended to limit the scope of the invention. It is also to be understood that the current system and method may be used to detect and identify other types of medical conditions, diseases and indicial thereof
[0039] The instant disease diagnosis approach starts with reading the user real time vital signs using a wearable sensor system. Any wearable sensor system known in the art are invention to be used in this invention. The wearable system may comprise one or more sensors. It is to be understood that any sensors known in the field for measuring parameters related to by way of non-limiting example to physiological, non-physiological, activity, motion and emotional data may be integrated into the wearable sensor system. In the current embodiment, two variables are introduced, the "control" to account for the sensor output range and whether it is normal or not and the "weighting factor" to determines the significant contribution of the corresponding sensor. These two parameters and the actual value of the sensor are used to determine an indicator value. The system then uses this "indicator" value to search a predefined disease look up table for the corresponding disease. This system helps in assessing the physical health of a person by providing diagnosis of possible diseases and checking treatment progress toward recovery. Using the instant system and algorithm, medical condition detection is faster than traditional techniques. That is, the present inventors observed the performance of calculating the health Indicator is faster 10% to 48% than the sequential search method.
A. System Architecture
[0040] In one embodiment, the present inventors developed a system architecture that permits medical condition detection based on an Indicator value within minimum or maximum ranges of a defined medical condition. For instance, and as illustrated in FIG. 1, an illustrative system architecture may have four stages: (a) Pre-Defined stage, (b) Pre-Processing Calculations, (c) Processing operations, and (d) Medical Condition' Detection. [0041] (a) Pre-Defined stage: in this stage, sensor ranges are setup with their corresponding minimum and maximum ranges. A weighting factor is defined as well as the medical conditions. [0042] (b) Pre-Processing Calculations: in this stage, the sensors values are captured and stored, and the minimum multiplication for each sensor is calculated using the weight factor (WF) defined from the previous stage. [0043] (c) Processing operations: in this stage a Control value is assigned for each sensor depending on whether its measured value is normal or abnormal. The control value is binary and therefor is either 0 or 1. In this stage, the Indicator factor will also be calculated based on: weight factor assigned to the sensor, the actual measurement of the sensor and the Control values. [0044] (d) Medical Condition' Detection: in this stage, the medical condition is detected based on the Indicator value being within the minimum or maximum ranges of the defined medical condition.
[0045] The system may perform operations that detect potential occurrences of, and compute indicia of several defined medical conditions. Usually a disease is constructed as a medical condition associated with specific symptoms and vital signs. Vital signs normally vary with, for example, age, weight, gender, and overall health. Measuring the vital signs for a person will provide an accurate figure about the body's physical status and the health condition. Due to the technological advancement of the biological sensor, presently there are dedicated sensors for each vital sign to capture the corresponding vital sign. Most human diseases are related to the status of the vital signs and whether their values are within or beyond the normal ranges. These vital signs are usually collected using dedicated sensors such as temperature, ECG, and breathing sensors. It is to be understood that these types of sensors are only exemplary and are not intended to limit the scope of the invention. So, it is to be understood that any sensors known in the art may be used in this invention for the purpose of measuring vital signs associated with, by way of non-limiting examples, physiological, non-physiological, activity, motional and emotional parameters. Also, while this application makes reference to the patient being a human in some instances, it is to be understood that such representation is only exemplary. It is also to be understood that a patient may cover any living organism from which vital signs may be obtained.
[0046] To accelerate development of a system architecture, the present inventors used a commercially available platform, namely e-Health Sensor Platform V2.0. The platform consists of 9 different wearable sensors which measure 11 vital signs and a shield to connect the sensors. FIG. 2 illustrates the sensors and the shield. Of course, it is understood that a similar platform could be used, and the present disclosure in no way requires a specific platform or commercial product. Also, while the current platform is shown to use 9 sensors and measure 11 vital signs, it is to be understood that this only exemplary and none limiting. In other embodiments, sensors ranging from 1 to n, where n is a natural number may be used. Similarly, other embodiment may be used to measure vital signs corresponding to any combination of all known vital signs.
[0047] While in no way limiting, Table 2 below provides a brief description of 9 sensors and the biometrics they measure. The present system measures 11 different biological signals. Those 11 signals have normal ranges that if a value outside the normal range has been detected, then the physiological status of the person is considered abnormal and then used to probably classify the patient as having a medical condition. The ranges for these signals change according to many factors such as, for example, age, gender, location etc. For example, heart rate normal ranges for an infant if he is awake is between 100 and 190 beats per minute (bpm) but while he is sleeping the range becomes 90 to 160 bpm. On the other hand, a sleeping adult normal heart rate is between 50 and 90 bpm but if he is awake the range becomes 60 to 100 bpm [25].
TABLE-US-00002 TABLE 2 Wearable Health Sensors and the biometric they measure The Sensor Biometric it measures Pulse and SPO2 sensor Heart Rate (HR) Arterial oxygen saturation (SPQ2) Airflow sensor Respiratory rates (RR) Body temperature sensor Body temperature (TEMP) (ECG) sensor Assess the electrical and muscular functions of the heart Glucometer Approximate concentration of glucose in the blood Sphygmomanometer Systolic blood pressure (SBP) Diastolic blood pressure (DBP) Galvanic skin response Measuring electrical conductance of the sensor (GSR) skin, which varies with its moisture level Accelerometer Patient positions Muscle/electromyography Electrical activity of muscles sensor (EMG)
[0048] The instant system may store, in one or more tangible, non-transitory memories, structured data records (e.g., within a lookup database) that act as reference and facilitate a detection of a particular medical condition based on biometric and other data captured by wearable devices in communication with the system across one or more communications networks. Such communication may be wired or wireless.
B. Medical Condition Detection
[0049] FIG. 3 describes a medical condition detection system according to an exemplary embodiment, which includes detecting a medical condition, or a disease from a list of defined medical conditions (diseases) based on the calculation of a variable called an Indicator. First, a disease must be identified. Second, the symptoms of the disease are specified. Third, the involved sensors sub ranges are defined. Forth, the maximum and the minimum value for the involved sensor are established and the corresponding control value for the involved sensors will be set to `1`. A weighting factor (WF) value is introduced. The weighting factor is a unique value assigned to each sensor. This value determines the significant contribution of the corresponding sensor. The WF value may vary from " 0" to " 1" . The weighting factor value corresponds to the frequency of use of a specific kind of sensor in several medical conditions in the look up table. In other words, for example, if there are 100 defined medical conditions based on 10 kind of sensors readings and the temperature is included in all of them, then its corresponding WF is 1, and if it is included in 85 conditions, its WF is 0.85 and so on and so forth. This factor will be used later in the computation of the "Indicator" value used to identify the corresponding medical condition. Since the WF depends on the total number of defined diseases in our database, every time we add a new disease we update the WF for the involved sensors. It is contemplated that with addition of more diseases to the look up table, the accuracy of to system will be enhanced. Fifth, the maximum and minimum "Indicator" value for the disease is computed and attached to the corresponding medical condition in the disease lookup table.
[0050] For instance and by way of non-limiting example, Table 3 below shows the weighting factors for some of the sensors used according to the defined medical conditions, consistent with the disclosed exemplary embodiments. In some aspects, certain of the disclosed systems may store one or more weighting factors in a corresponding database. The weighting factors numbers assigned to different type of sensors are listed in Table 3.
TABLE-US-00003 TABLE 3 Sample of the used sensors with their corresponding weighting factor WFS Sensor Type sensor Abbreviation 0.7 Heart Rate Sensor HR_SENSOR 0.9 Blood Pressure Sensor BP_SENSOR 0.2 Spo2 Sensor SPO2_SENSOR 0.6 Temperature SENSOR TEMP_SENSOR 0.5 Respiration Rate Sensor RR_SENSOR 0.2 Glucose Level SENSOR GLOCOSE_SENSOR
[0051] It is noted that each sensor has a sensing range. This sensing range could be divided into small ranges. As an example, Table 4 below presents the sub ranges for human temperature sensor's reading as a non-limiting example. In this example, the sensor has four (4) intervals each with its corresponding range values. When body temperature falls below 35.0.degree. C., the subject has hypothermia. Hypothermia is a medical emergency that occurs when human's body loses heat faster than it can produce heat, causing a dangerously low body temperature. The normal range of internal human body temperature varies between (36.5-37.5).degree. C.
TABLE-US-00004 TABLE 4 Defined human temperature classification ranges [27][28][29][30][31] Ranges Symptom Interval STR1 Hypothermia <35.0.degree. C. (95.0.degree. F.) STNR Normal 36.5-37.5.degree. C. (97.7-99.5.degree. F.) STR2 Fever >37.5 or 38.3.degree. C. (99.5 or 100.9.degree. F.) STR4 Hyperpyrexia >40.0 or 41.5.degree. C. (104.0 or 106.7.degree. F.)
"Indicator" Computational Algorithm
[0052] As stated previously, the proposed system starts whenever subject sensors measurements are available. For each sensor, three parameters were defined, namely their WF, minimum and maximum values. The proposed system then uses these values to compute the corresponding minimum and maximum range values of the "Indicator" parameter. Table 4 is updated by adding to it a new column that represents the actual measured value. If the actual measured value lies in the normal range, the corresponding control value is set to "0", otherwise, it is set to "1". Based on this, if all the sensors readings are within their normal ranges, then the `Indicator` value will be "0", thus no medical condition is detected (diseases free case). Table 5 shows the indicator computation matrix.
TABLE-US-00005 TABLE 5 Indicator computation matrix Sensor rule WF Min Max Actual Control S1R WF1 Mini Maxi A1 C1 = "0" or "1" S2R WF2 Min2 Max2 A2 C2 = "0" or "1" S3R WF3 Min3 Max3 A3 C3 = "0" or "1" S4R WF4 Min4 Max4 A4 C4 = "0" or "1" S5R WF5 Min5 Max5 A5 C5 = "0" or "1" S6R WF6 Min6 Max6 A6 C6 = "0" or "1" S7R WF7 Min7 Max7 A7 C7 = "0" or "1"
[0053] The developed algorithm is used to determine the "Indicator" and its minimum and maximum interval values. The system then uses this Indicator value to search a look up table for the corresponding disease. The Indicator for a specific disease is computed using the below formula:
Indicator=.SIGMA..sub.i=1.sup.n (WF.sub.i)(A.sub.i)(C.sub.i) (1)
and the corresponding minimum (Min_Ind) and maximum (Max_Ind) for the indicator values for a specific disease are computed using the following equations:
Min_Ind=.SIGMA..sub.i=1.sup.n (WF.sub.i)(Min.sub.i)(C.sub.i) (2)
Max_Ind =.SIGMA..sub.i=1.sup.n (WF.sub.i)(Max.sub.i)(C.sub.i) (3)
where WF.sub.i, A.sub.i, C.sub.i, Min.sub.i, Max.sub.i, and i are the weighting factor, actual reading of the sensor, control, minimum, maximum range values, and the number of the sensor, respectively and where n is a natural number.
[0054] The Min_Ind and the Max_Ind values are computed and saved in a disease lookup table. Each disease has an interval to identify it and this interval is defined by the Min_Ind and the Max_Ind values. Every time a new disease is added to a database, its `Indicator` interval is defined using equations 2 and 3. The disease lookup table is implemented as a binary search tree (BST). The BST facilitate and accelerate the range search process.
[0055] In some embodiments, the look up table may be populated with entries related to emotional conditions, diseases or abnormalities. In such embodiments, the system and method of the current disclosure may be used to identify and detect emotional states, conditions, diseases disorders and/or abnormalities based on the measured sensor data and the developed algorithm. Some examples of the above may include but is not limited to sadness, happiness, anger, excitement, mania, depression and other emotional conditions known in the art.
Exemplary Computer-Implemented Processes for Automatic Disease Detection
[0056] The detailed disease diagnosis overview is shown in FIG. 4. First, the uservital signs readings are provided to the system. The sensors whose readings are in the normal range, their index (control) value will be set to zero and the other sensors control value will be set to 1. Then, the `Indicator` value is computed from the actual sensor reading value, the sensor control value and the sensor weight factor value. If the computed `Indicator` value equals zero then the user's vital signs are in the normal range but if the `Indicator` value is greater than zero, this means that the user is suffering from a specific disease. The `Indicator` value is then used by the processor to search the disease lookup table for the corresponding disease and to present it as a suggested diagnosis.
[0057] In no way limiting and as an example, Table 6 below shows the structure of the disease lookup table for four medical conditions. As revealed through equations (2) and (3), the calculation of the corresponding disease's minimum and maximum "Indicator" values is independent of the actual real time sensor reading. Indeed, all parameters used for determining Min_Ind and Max_Ind are predefined values.
TABLE-US-00006 TABLE 6 Disease lookup table for diagnosis and identification. Disease Min_Ind Max_Ind MCI Min_Ind1 Max_Ind1 MC2 Min_Ind2 Max_Ind2 MC3 Min_Ind3 Max_Ind3 MC4 Min_Ind4 Max_Ind4
[0058] The instant system does not require any medical information to be provided and entered by the user manually. Rather, all what is needed is to connect the sensors to the subject's body. This may require a one-time training for the user to teach him/her where and how to place the sensors. In some embodiments where sensors may be placed in wearables such as watches, fit bits, health bracelets or the like, the subject's initial training for placement of the sensors may not be required. The instant system, and certain exemplary computer-implemented processes described above, may be implement in addition to, or as an alternate to, known web-based medical diagnostic tools where the user needs to type his symptoms manually. In such traditional systems described in the prior art, it is required that the patient knows the medical terms for the symptoms he or she is experiencing and their correct spelling. Also, in such traditional known system and diagnostic tools, identification of a symptomless diseases, such as Hypertension, would not be possible. The current invention is advantageous over such traditional known online diagnostic systems and tools because it is able to overcome both of these deficiencies. By allowing the system to rely only on data obtained from the sensors, the system is able to work passively and eliminate subjectivity of the patient or physician. Also, by using sensors that are able to collect data continuously, such as wearables, the system may be considered a continuous monitoring system.
[0059] The process of detecting diseases using the new algorithm is depicted as a pseudocode and is exemplified in FIG. 5.
EXAMPLES
System Testing and Evaluation
[0060] In order to demonstrate the applicability of the instant system and algorithm in real life situations, the inventors developed the main functions and components and performed various experimental tests. After that, the inventors conducted several measurements to evaluate the system' s performance.
[0061] It is understood that the below Examples are illustrative and non-limiting. It will, however, be evident that various modifications and changes may be made thereto, and additional embodiments may be implemented, without departing from the broader scope of the disclosed embodiments.
Example 1
System Testing Setup
[0062] To validate the instant eHealth architecture and disease detection algorithm, the inventors developed a test bench, as shown in FIG. 6. The test bench has three elements: wearable Bluetooth sensors simulator, the medical gateway, and the eHealth remote server.
[0063] The simulator enables the simulation of various medical sensors output. This simulator may be installed on a tablet. In the actual system, the simulator may be replaced by a set of wearable medical sensors mounted on the patient (as depicted in FIG. 2). Digital values of vital signs are sent from the simulator to the medical gateway using Bluetooth low energy wireless network technology. Other means of wireless or wired communication may be used. The medical gateway (an application running on a smart tablet or other processor or smart device) collects vital signs and displays them in real time on a display; at the same time these values are transferred to an eHealth server for further analysis and disease detection. The eHealth server analyzes vital signs values using the instant algorithm for disease detection as explained above. Once a disease or some symptoms have been detected, the server sends a notification to the patient, (this notification will be displayed in real time on the display of the tablet or other device) and an email alert will be sent to the doctor. In some embodiments, other forms of notifications may also be triggered. For example, notification may be provided to the patient in the form of audio or visual notification. It may also be sent to the patient's email or by form of text message to his mobile. Notification may also be sent to the hospital or an emergency contact of the subject or an emergency mobile unit depending on the severity of the condition or disease identified and based on pre-set instructions for such notification by the user.
[0064] In this specific example, a software simulator with a set of virtual wearable sensors was designed to setup a specific medical condition. The simulator set of virtual sensors' output is adjustable and can be manipulated to correspond to a specific disease.
[0065] FIG. 7 provides an exemplary designed simulator. This hybrid simulator sensors configuration framework is developed to simulate continuous dynamics of the human's physiology. The medical conditions can be simulated by adjusting the slider to a certain value. A decision was made during the conducted experiments to only use the first seven sensors. The remaining sensors may be activated whenever there is a need. The listed medical conditions in Table 1 may be simulated by configuring the first seven sensors only and the simulator can be updated to include further type of sensors.
[0066] Different communication protocols are used to transmit the collected data to the storage and processing servers, i.e. Bluetooth Smart Ready and WiFi. The Bluetooth protocol was used because of its short-range connectivity, low power consumption, high connectivity bandwidth and its lightweight receiver/transmitter load. While the WiFi protocol was used to connect the gateway with the cloud servers via the internet due to its liability, and wide-range (approx. 50 m) connectivity, the cloud environment was chosen due to its availability, huge processing capabilities as well as its large storage resources. The test bed for the experimental setup is depicted in FIG. 8. The purpose of the experiment is to evaluate the performance of the instant algorithm in detecting the medical conditions. Those tests should demonstrate the efficiency of the instant algorithm in comparison with conventional and linear algorithms. The experiments should also evaluate system performance in terms of the data transfer rate and computational time.
Example 2
Bluetooth Data Transfer Time
[0067] FIG. 9 displays the data transfer from the sensors simulator (Peripheral Device) to the medical gateway (called Central). The peripheral has an advertisement interval of 300 milliseconds (ms), however the advertisement time was fixed by the software to 100 ms. The Central has a scan window of 50 ms and a scan interval of 100 ms. Of course, it is understood that this is a non-limiting example.
Example 3
[0068] Data Transfer from Gateway to Server
[0069] The second test will evaluate the data transfer time needed for sending data from the medical gateway to a server. The result are depicted in FIG. 10 and it shows an average of 155 milliseconds. The x axis represents number of tests run and the y axis represent the time in milliseconds.
Example 4
Testing Disease Detection Algorithm
[0070] The last test was mainly designed to evaluate the performance and efficiency of the instant algorithm to detect disease. To measure the time required for disease detection a custom script was created, similar to the one executed on eHealth server to measure the differences between the proposed algorithm and any conventional algorithm using searching in a normal lookup table sequential as shown in the pseudocode below in FIG. 11.
[0071] The script includes measurement functions that measures the times required to execute the following tasks: [0072] eHealth Indicator calculation time. Disease search time in the lookup table. [0073] Disease total detection time using eHealth Indicator and lookup table. [0074] Disease detection time using the conventional sequential algorithm (vital signs are compared with the normal and abnormal ranges of each sensor)
TABLE-US-00007 [0074] TABLE 7 Summary of the computation time lapsed, obtain from the different tests (time in seconds) Disease Disease eHealth Time to Detection detection Delta Indicator search time time using time % eHealth Calc. disease using sequential .DELTA. = (D * TEST Indicator time in lookup Indicator test 100/C) - N.sup.o value (A) (B) C = A + B (D) 100 Detected diseases 1 376.900 0.000898 0.00015800 0.001056 0.001527 44.63% Severe Hypertension 2 48.500 0.000786 0.00011500 0.000901 0.001184 31.42% Hypotension/Diabetes/ Moderate Hypertension 3 176.400 0.000786 0.00011500 0.000901 0.001184 31.42% Asthma Severe/ Moderate Hypertension 4 189.200 0.000816 0.00021900 0.001035 0.001165 12.53% Asthma Severe/ Moderate Hypertension 5 0.000 0.001005 0.00015300 0.001158 0.001534 32.43% No disease detection 6 111.400 0.000473 0.00008300 0.000556 0.000795 43.04% Tachycardia/Asthma Severe/Moderate Hypertension 7 132.300 0.000804 0.00014800 0.000952 0.001305 37.10% Tachycardia/Asthma Severe/Moderate Hypertension 8 21.700 0.000816 0.00021900 0.001035 0.001165 12.53% Bradycardia/ Hypotension/ Respiratory Arrest Imminent/Moderate Hypertension 9 35.000 0.000688 0.00014500 0.000833 0.001235 48.26% Bradycardia/ Hypotension/Pre diabetes/Respiratory Arrest Imminent/ Moderate Hypertension 10 111.300 0.000898 0.00018400 0.001082 0.001252 15.69% Tachycardia/Asthma Severe/Moderate Hypertension 11 133.000 0.002494 0.00012700 0.002621 0.002945 12.37% Tachycardia/Asthma Severe/Moderate Hypertension 12 221.000 0.000461 0.00007900 0.000540 0.000632 17.09% Moderate Hypertension 13 53.800 0.000868 0.00024200 0.001110 0.001351 21.67% Hypotension/Diabetes/ Moderate Hypertension 14 64.200 0.000919 0.00015000 0.001069 0.001561 46.00% Hypotension/Diabetes/ Moderate Hypertension 15 94.800 0.000847 0.00015600 0.001003 0.001403 39.93% Tachycardia/Asthma Moderate/Moderate Hypertension 16 71.400 0.000873 0.00019300 0.001066 0.001245 16.80% Tachycardia/ Hypotension/Diabetes/ Moderate Hypertension 17 30.500 0.000889 0.00019500 0.001084 0.001554 43.32% Bradycardia/ Hypotension/Pre diabetes/Respiratory Arrest Imminent/ Moderate Hypertension 18 376.900 0.000994 0.00019600 0.001190 0.001434 20.49% Severe Hypertension 19 48.500 0.000899 0.00016300 0.001062 0.001190 12.02% Hypotension/Diabetes/ Moderate Hypertension 20 21.700 0.000559 0.00010300 0.000662 0.000733 10.66% Bradycardia/ Hypotension/ Respiratory Arrest Imminent/Moderate Hypertension 21 166.500 0.000873 0.00019300 0.001066 0.001245 16.80% Asthma Severe/ Moderate Hypertension 22 8.800 0.005223 0.00020700 0.005430 0.006163 13.49% Bradycardia/ Hypotension/ Hypoxaemia/Tachypnea/ Moderate Hypertension 23 195.300 0.000780 0.00013800 0.000918 0.001296 41.15% Asthma Severe/ Moderate Hypertension 24 241.300 0.001247 0.00021000 0.001457 0.001674 14.89% Moderate Hypertension 25 221.000 0.000461 0.00007900 0.000540 0.000775 43.43% Moderate Hypertension 26 221.000 0.000878 0.00015100 0.001029 0.001284 24.74% Moderate Hypertension 27 264.600 0.000878 0.00015100 0.001029 0.001284 24.74% Severe Hypertension
[0075] The comparison chart shown below (FIG. 12) shows the disease detection time using the eHealth Indicator and the lookup table. It is clear that the instant algorithm is much faster than the conventional algorithm using the sequential test. The instant algorithm uses an access to the database in order to get real-time vital signs and to check the medical conditions. The calculation time change depending on the server load. Therefore, the tests were conducted on a dedicated local host instead of cloud-based server to avoid the server load factor. During all the tests conducted, it was observed that the performance of the method and system used in the instant algorithm for calculating the health Indicator is faster 10.66% to 48.26% than the sequential search method.
[0076] Compared to the conventional linear search (sequential search) method for finding the target rule in a list and trigger its action, the sequential search method checks each and every rule in the list until it finds the matching rule or all the rules are searched without finding a match. An online tool has been developed to test the instant algorithm's performance on real-time in detecting the diseases and improve the performance as fast as possible. FIG. 13 provides a screenshot of the online test.
[0077] For example, to detect a " Severe Hypertension" by both algorithms based on the given vital signs by the sensors, the sequential " Serial" search algorithm elapsed 173 milliseconds to detect the disease, while the Indicator algorithm lapsed only 129 milliseconds to detect the same. This raises the performance of the diagnostic system and method to up to 34% for this particular medical condition. Further examples of diagnostic indicators are shown in Table 8.
TABLE-US-00008 TABLE 8 Further examples of diagnostic indicators Disease Description Vital signs ranges Associated sensor/s Bradycardia abnormally slow heart rate <60 beats/min HR_SENSOR Tachycardia abnormally fast heart rate >100 OR > 120 beats/min HR_SENSOR Hypotension abnormally low blood pressure BP < 100 mm Hg systolic BP_SENSOR Hypertension abnormally high blood pressure Mild to moderate (systolic BP_SENSOR blood pressure < 180 mm Hg and diastolic blood pressure below 110 mm Hg) Severe hypertension, BP_SENSOR defined as a systolic pressure > 180 mm Hg or diastolic pressure > 110 mm Hg, Hypoxaemia abnormally low concentration of oxygen SP02 < 95% SP02_SENSOR in the blood Hyperthermia abnormally high body temperature core temperature > 37.80.degree. C. TEMP_SENSOR Hypothermia Abnormally low body temperature core temperature < 36.0.degree. C. TEMP_SENSOR Bradypnea abnormally slow breathing rate RR < 20 breaths/min RR_SENSOR Tachypnea abnormally fast breathing rate RR > 25 breaths/min RR_SENSOR Sinus P waves are hidden within each preceding ECG image "camel hump" ECG_SENSOR Tachycardia T wave appearance Prediabetes blood sugar level is higher than normal Fasting glucose level: GLOCOSE_SENSOR but not yet high enough to be classified as (100-125) (mg/dL) type 2 diabetes Diabetes describes a group of metabolic diseases in Fasting glucose level: GLOCOSE_SENSOR which the person has high blood glucose more than 125 (mg/dL) (blood sugar), either because insulin production is inadequate, or because the body's cells do not respond properly to insulin, or both Pneumonia a disease of the lungs characterized RR > 25 breaths/min RR_SENSOR especially by inflammation and HR > 100 OR HR > 120 beats/min HR_SENSOR consolidation of lung tissue followed by core temperature > 37.80.degree. C. TEMP_SENSOR resolution and by fever, chills, cough, and difficulty in breathing and that is caused especially by infection Urosepsis is a systemic reaction of the body (SIRS) core temperature > 37.80.degree. C. TEMP_SENSOR to a bacterial infection of the urogenital HR > 100 or HR > 120 beats/min HR_SENSOR organs with the risk of life-threatening BP < 100 mm Hg systolic BP_SENSOR symptoms including shock Asthma is a chronic inflammatory disorder of the 90% < SPO2 < 95% SP02_SENSOR Moderate airways 100 < HR < 120 beats/min HR_SENSOR RR > 25 breaths/min RR_SENSOR Asthma is sever chronic inflammatory disorder of SP02 < 90% SP02_SENSOR Severe the airways HR > 120 beats/min HR_SENSOR RR > 25 breaths/min RR_SENSOR Respiratory is the cessation of normal breathing due SP02 < 90% SP02_SENSOR Arrest to failure of the lungs to function effectively HR < 60 beats/min HR_SENSOR Imminent RR > 30 breaths/min RR_SENSOR
Exemplary Hardware and Software Implementations
[0078] Embodiments of the subject matter and the functional operations described in this specification can be implemented in digital electronic circuitry, in tangibly-embodied computer software or firmware, in computer hardware, including the structures disclosed in this specification and their structural equivalents, or in combinations of one or more of them. Embodiments of the subject matter described in this specification, can be implemented as one or more computer programs, i.e., one or more modules of computer program instructions encoded on a tangible non transitory program carrier for execution by, or to control the operation of, data processing apparatus. Additionally or alternatively, the program instructions can be encoded on an artificially generated propagated signal, such as a machine-generated electrical, optical, or electromagnetic signal that is generated to encode information for transmission to suitable receiver apparatus for execution by a data processing apparatus. The computer storage medium can be a machine-readable storage device, a machine-readable storage substrate, a random or serial access memory device, or a combination of one or more of them.
[0079] The term "data processing apparatus" refers to data processing hardware and encompasses all kinds of apparatus, devices, and machines for processing data, including by way of example a programmable processor, a computer, or multiple processors or computers. The apparatus can also be or further include special purpose logic circuitry, such as an FPGA (field programmable gate array) or an ASIC (application specific integrated circuit). The apparatus can optionally include, in addition to hardware, code that creates an execution environment for computer programs, such as code that constitutes processor firmware, a protocol stack, a database management system, an operating system, or a combination of one or more of them.
[0080] A computer program, which may also be referred to or described as a program, software, a software application, a module, a software module, a script, or code, can be written in any form of programming language, including compiled or interpreted languages, or declarative or procedural languages, and it can be deployed in any form, including as a stand alone program or as a module, component, subroutine, or other unit suitable for use in a computing environment. A computer program may, but need not, correspond to a file in a file system. A program can be stored in a portion of a file that holds other programs or data, such as one or more scripts stored in a markup language document, in a single file dedicated to the program in question, or in multiple coordinated files, such as files that store one or more modules, sub programs, or portions of code. A computer program can be deployed to be executed on one computer or on multiple computers that are located at one site or distributed across multiple sites and interconnected by a communication network.
[0081] The processes and logic flows described in this specification can be performed by one or more programmable computers executing one or more computer programs to perform functions by operating on input data and generating output. The processes and logic flows can also be performed by, and apparatus can also be implemented as, special purpose logic circuitry, such as an FPGA (field programmable gate array) or an ASIC (application specific integrated circuit).
[0082] Computers suitable for the execution of a computer program include, by way of example, general or special purpose microprocessors or both, or any other kind of central processing unit. Generally, a central processing unit will receive instructions and data from a read only memory or a random access memory or both. The essential elements of a computer are a central processing unit for performing or executing instructions and one or more memory devices for storing instructions and data. Generally, a computer will also include, or be operatively coupled to receive data from or transfer data to, or both, one or more mass storage devices for storing data, such as magnetic, magneto optical disks, or optical disks. However, a computer need not have such devices. Moreover, a computer can be embedded in another device, such as a mobile telephone, a personal digital assistant (PDA), a mobile audio or video player, a game console, a Global Positioning System (GPS) receiver, or a portable storage device, such as a universal serial bus (USB) flash drive, to name just a few.
[0083] Computer readable media suitable for storing computer program instructions and data include all forms of non-volatile memory, media and memory devices, including by way of example semiconductor memory devices, such as EPROM, EEPROM, and flash memory devices; magnetic disks, such as internal hard disks or removable disks; magneto optical disks; and CD ROM and DVD-ROM disks. The processor and the memory can be supplemented by, or incorporated in, special purpose logic circuitry.
[0084] To provide for interaction with a user, embodiments of the subject matter described in this specification can be implemented on a computer having a display device, such as a CRT (cathode ray tube) or LCD (liquid crystal display) monitor, for displaying information to the user and a keyboard and a pointing device, such as a mouse or a trackball, by which the user can provide input to the computer. Other kinds of devices can be used to provide for interaction with a user as well; for example, feedback provided to the user can be any form of sensory feedback, such as visual feedback, auditory feedback, or tactile feedback; and input from the user can be received in any form, including acoustic, speech, or tactile input. In addition, a computer can interact with a user by sending documents to and receiving documents from a device that is used by the user; for example, by sending web pages to a web browser on a user' s device in response to requests received from the web browser.
[0085] Implementations of the subject matter described in this specification can be implemented in a computing system that includes a back end component, such as a data server, or that includes a middleware component, such as an application server, or that includes a front end component, such as a client computer having a graphical user interface or a Web browser through which a user can interact with an implementation of the subject matter described in this specification, or any combination of one or more such back end, middleware, or front end components. The components of the system can be interconnected by any form or medium of digital data communication, such as a communication network. Examples of communication networks include a local area network (LAN) and a wide area network (WAN), such as the Internet.
[0086] The computing system can include clients and servers. A client and server are generally remote from each other and typically interact through a communication network. The relationship of client and server arises by virtue of computer programs running on the respective computers and having a client-server relationship to each other. In some implementations, a server transmits data, such as an HTML page, to a user device, such as for purposes of displaying data to and receiving user input from a user interacting with the user device, which acts as a client. Data generated at the user device, such as a result of the user interaction, can be received from the user device at the server.
[0087] While this specification contains many specifics, these should not be construed as limitations, but rather as descriptions of features specific to particular embodiments. Certain features that are described in this specification in the context of separate embodiments may also be implemented in combination in a single embodiment. Conversely, various features that are described in the context of a single embodiment may also be implemented in multiple embodiments separately or in any suitable sub-combination. Moreover, although features may be described above as acting in certain combinations and even initially claimed as such, one or more features from a claimed combination may in some cases be excised from the combination, and the claimed combination may be directed to a sub-combination or variation of a sub-combination.
[0088] Similarly, while operations are depicted in the drawings in a particular order, this should not be understood as requiring that such operations be performed in the particular order shown or in sequential order, or that all illustrated operations be performed, to achieve desirable results. In certain circumstances, multitasking and parallel processing may be advantageous. Moreover, the separation of various system components in the embodiments described above should not be understood as requiring such separation in all embodiments, and it should be understood that the described program components and systems may generally be integrated together in a single software product or packaged into multiple software products.
[0089] In each instance where an HTML file is mentioned, other file types or formats may be substituted. For instance, an HTML file may be replaced by an XML, JSON, plain text, or other types of files. Moreover, where a table or hash table is mentioned, other data structures (such as spreadsheets, relational databases, or structured files) may be used.
[0090] While this specification contains many specifics, these should not be construed as limitations, but rather as descriptions of features specific to particular implementations. Certain features that are described in this specification in the context of separate implementations may also be implemented in combination in a single implementation. Conversely, various features that are described in the context of a single implementation may also be implemented in multiple implementations separately or in any suitable sub-combination. Moreover, although features may be described above as acting in certain combinations and even initially claimed as such, one or more features from a claimed combination may in some cases be excised from the combination, and the claimed combination may be directed to a sub-combination or variation of a sub-combination.
[0091] Similarly, while operations are depicted in the drawings in a particular order, this should not be understood as requiring that such operations be performed in the particular order shown or in sequential order, or that all illustrated operations be performed, to achieve desirable results. In certain circumstances, multitasking and parallel processing maybe advantageous. Moreover, the separation of various system components in the implementations described above should not be understood as requiring such separation in all implementations, and it should be understood that the described program components and systems may generally be integrated together in a single software product or packaged into multiple software products.
[0092] Various embodiments have been described herein with reference to the accompanying drawings. It will, however, be evident that various modifications and changes may be made thereto, and additional embodiments may be implemented, without departing from the broader scope of the disclosed embodiments.
[0093] Further, other embodiments will be apparent to those skilled in the art from consideration of the specification and practice of one or more embodiments of the present disclosure. It is intended, therefore, that this disclosure and the examples herein be considered as exemplary only.
Interpretation of Terms
[0094] Unless the context clearly requires otherwise, throughout the description and the claims: [0095] "comprise," "comprising," and the like are to be construed in an inclusive sense, as opposed to an exclusive or exhaustive sense; that is to say, in the sense of "including, but not limited to". [0096] "connected," "coupled," or any variant thereof, means any connection or coupling, either direct or indirect, between two or more elements; the coupling or connection between the elements can be physical, logical, or a combination thereof. [0097] "patient", "subject" or "user" or any variations thereof refers to any recipient of healthcare services. [0098] "physiological data" refers to data associated with physiological parameters of the patient. The physiological parameters include, but not limited to, body temperature, hearth rate, body exhilaration and respiration rate. [0099] "herein," "above," "below," and words of similar import, when used to describe this specification shall refer to this specification as a whole and not to any particular portions of this specification. [0100] "or," in reference to a list of two or more items, covers all of the following interpretations of the word: any of the items in the list, all of the items in the list, and any combination of the items in the list. [0101] the singular forms "a", "an" and "the" also include the meaning of any appropriate plural forms.
[0102] Words that indicate directions such as "vertical", "transverse", "horizontal", "upward", "downward", "forward", "backward", "inward", "outward", "vertical", "transverse", "left", "right", "front", "back", "top", "bottom", "below", "above", "under", "upper", "lower" and the like, used in this description and any accompanying claims (where present) depend on the specific orientation of the apparatus described and illustrated. The subject matter described herein may assume various alternative orientations. Accordingly, these directional terms are not strictly defined and should not be interpreted narrowly.
[0103] Where a component (e.g. a circuit, module, assembly, device, etc.) is referred to above, unless otherwise indicated, reference to that component (including a reference to a "means") should be interpreted as including as equivalents of that component any component which performs the function of the described component (i.e., that is functionally equivalent), including components which are not structurally equivalent to the disclosed structure which performs the function in the illustrated exemplary embodiments of the invention.
[0104] Specific examples of device and method have been described herein for purposes of illustration. These are only examples. The technology provided herein can be applied to system and method other than the examples described above. Many alterations, modifications, additions, omissions and permutations are possible within the practice of this invention. This invention includes variations on described embodiments that would be apparent to the skilled addressee, including variations obtained by: replacing features, elements and/or acts with equivalent features, elements and/or acts; mixing and matching of features, elements and/or acts from different embodiments; combining features, elements and/or acts from embodiments as described herein with features, elements and/or acts of other technology; and/or omitting combining features, elements and/or acts from described embodiments.
[0105] It is therefore intended that the following appended claims and claims hereafter introduced are interpreted to include all such modifications, permutations, additions, omissions and sub-combinations as may reasonably be inferred. The scope of the claims should not be limited by the preferred embodiments set forth in the examples, but should be given the broadest interpretation consistent with the description as a whole.
* * * * *
D00000
D00001
D00002
D00003
D00004

D00005

D00006

D00007

D00008
D00009

D00010
D00011
D00012
XML
uspto.report is an independent third-party trademark research tool that is not affiliated, endorsed, or sponsored by the United States Patent and Trademark Office (USPTO) or any other governmental organization. The information provided by uspto.report is based on publicly available data at the time of writing and is intended for informational purposes only.
While we strive to provide accurate and up-to-date information, we do not guarantee the accuracy, completeness, reliability, or suitability of the information displayed on this site. The use of this site is at your own risk. Any reliance you place on such information is therefore strictly at your own risk.
All official trademark data, including owner information, should be verified by visiting the official USPTO website at www.uspto.gov. This site is not intended to replace professional legal advice and should not be used as a substitute for consulting with a legal professional who is knowledgeable about trademark law.