System and method for treating the structure of the human lens with a laser
Frey , et al. November 24, 2
U.S. patent number 10,842,675 [Application Number 11/337,127] was granted by the patent office on 2020-11-24 for system and method for treating the structure of the human lens with a laser. This patent grant is currently assigned to Lensar, Inc.. The grantee listed for this patent is Rudolph W. Frey, Gary P. Gray, Jerome Kuszak, Dennis R. Pape. Invention is credited to Rudolph W. Frey, Gary P. Gray, Jerome Kuszak, Dennis R. Pape.











View All Diagrams
| United States Patent | 10,842,675 |
| Frey , et al. | November 24, 2020 |
System and method for treating the structure of the human lens with a laser
Abstract
A system and method for increasing the amplitude of accommodation and/or changing the refractive power and/or enabling the removal of the clear or cataractous lens material of a natural crystalline lens is provided. Generally, the system comprises a laser, optics for delivering the laser beam and a control system for delivering the laser beam to the lens in a particular pattern. There is further provided a device for determining the shape and position of the lens with respect to the laser. There is yet further provided a method and system for delivering a laser beam in the lens of the eye in a predetermined shot pattern that utilize as series of shots that form a shell cut, a partial shell cut, a laser suture cut and/or a volumetric shaped removal, which essentially following the shape of a suture layer of the lens.
| Inventors: | Frey; Rudolph W. (Maitland, FL), Gray; Gary P. (Orlando, FL), Pape; Dennis R. (Orlando, FL), Kuszak; Jerome (Oak Park, IL) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Applicant: |
|
||||||||||
| Assignee: | Lensar, Inc. (Orlando,
FL) |
||||||||||
| Family ID: | 1000005199813 | ||||||||||
| Appl. No.: | 11/337,127 | ||||||||||
| Filed: | January 20, 2006 |
Prior Publication Data
| Document Identifier | Publication Date | |
|---|---|---|
| US 20070173794 A1 | Jul 26, 2007 | |
| Current U.S. Class: | 1/1 |
| Current CPC Class: | A61F 9/00834 (20130101); A61F 9/008 (20130101); A61B 90/30 (20160201); A61F 2009/00897 (20130101); A61F 9/00736 (20130101); A61B 90/361 (20160201); A61F 2009/0087 (20130101); A61B 2018/20355 (20170501); A61B 2018/20351 (20170501); A61F 2009/00887 (20130101); A61B 2018/20361 (20170501) |
| Current International Class: | A61F 9/008 (20060101); A61B 90/30 (20160101); A61B 90/00 (20160101); A61B 18/20 (20060101); A61F 9/007 (20060101) |
References Cited [Referenced By]
U.S. Patent Documents
| 3074407 | January 1963 | Moon et al. |
| 3971382 | July 1976 | Krasnov |
| 3982541 | September 1976 | L'Esperance, Jr. |
| 4024852 | May 1977 | L'Esperance et al. |
| 4263893 | April 1981 | Pavlak et al. |
| 4309998 | January 1982 | Aron nee Rosa et al. |
| 4334736 | June 1982 | Herbert |
| 4381007 | April 1983 | Doss |
| 4394144 | July 1983 | Aoki |
| 4461294 | July 1984 | Baron |
| 4477159 | October 1984 | Mizuno et al. |
| 4502816 | March 1985 | Creter, Jr. et al. |
| 4517980 | May 1985 | Tagnon |
| 4538608 | September 1985 | L'Esperance |
| 4554917 | November 1985 | Tagnon |
| 4561436 | December 1985 | Munnerlyn |
| 4565197 | January 1986 | Daly |
| 4573193 | February 1986 | Shuto et al. |
| 4573778 | March 1986 | Shapiro |
| 4576160 | March 1986 | Tanaka |
| 4579430 | April 1986 | Bille |
| 4580559 | April 1986 | L'Esperance |
| 4582405 | April 1986 | Muller et al. |
| 4583539 | April 1986 | Karlin et al. |
| 4588505 | May 1986 | Walley et al. |
| 4601037 | July 1986 | McDonald |
| 4601288 | July 1986 | Myers |
| 4607622 | August 1986 | Fritch et al. |
| 4628416 | December 1986 | Dewey |
| 4633866 | January 1987 | Peyman et al. |
| 4638801 | January 1987 | Daly et al. |
| 4644948 | February 1987 | Lang et al. |
| 4648400 | March 1987 | Schneider et al. |
| 4657013 | April 1987 | Hoerenz et al. |
| 4665913 | May 1987 | L'Esperance, Jr. |
| 4669466 | June 1987 | L'Esperance, Jr. |
| 4669839 | June 1987 | Muchel |
| 4682595 | July 1987 | Hoerenz et al. |
| 4686979 | August 1987 | Gruen et al. |
| 4686992 | August 1987 | Dewey et al. |
| 4702245 | October 1987 | Schroder et al. |
| 4702576 | October 1987 | Magnante |
| 4711540 | December 1987 | Yoshino et al. |
| 4711541 | December 1987 | Yoshino et al. |
| 4712543 | December 1987 | Baron |
| 4715703 | December 1987 | Cornsweet et al. |
| 4718418 | January 1988 | L'Esperance, Jr. |
| 4719912 | January 1988 | Wienberg |
| 4721379 | January 1988 | L'Esperance |
| 4724522 | February 1988 | Belgorod |
| 4729372 | March 1988 | L'Esperance, Jr. |
| 4729373 | March 1988 | Peyman |
| 4732148 | March 1988 | L'Esperance, Jr. |
| 4732460 | March 1988 | Kele et al. |
| 4736744 | April 1988 | Koike et al. |
| 4741612 | May 1988 | Birngruber et al. |
| 4744362 | May 1988 | Grundler |
| 4758081 | July 1988 | Barnes |
| 4764930 | August 1988 | Bille |
| 4765336 | August 1988 | Blaha et al. |
| 4770162 | September 1988 | L'Esperance et al. |
| 4770172 | September 1988 | L'Esperance, Jr. |
| 4770486 | September 1988 | Wang et al. |
| 4772116 | September 1988 | Schroder et al. |
| 4773414 | September 1988 | L'Esperance, Jr. |
| 4775361 | October 1988 | Jacques et al. |
| 4776687 | October 1988 | Nakanishi et al. |
| 4798204 | January 1989 | L'Esperance, Jr. |
| 4820264 | April 1989 | Matsui et al. |
| 4830483 | May 1989 | Kohayakawa et al. |
| 4832043 | May 1989 | Ichihashi |
| 4837857 | June 1989 | Scheller et al. |
| 4838266 | June 1989 | Koziol et al. |
| 4840175 | June 1989 | Peyman |
| 4846172 | July 1989 | Berlin |
| 4848340 | July 1989 | Bille et al. |
| 4854693 | August 1989 | Ichihashi et al. |
| 4856513 | August 1989 | Muller |
| 4862888 | September 1989 | Yessik |
| 4863261 | September 1989 | Flammer |
| 4865029 | September 1989 | Pankratov |
| 4865441 | September 1989 | Reis |
| 4866243 | September 1989 | Sakane et al. |
| 4870952 | October 1989 | Martinez |
| 4881808 | November 1989 | Bille et al. |
| 4883351 | November 1989 | Weiss |
| 4884884 | December 1989 | Reis |
| 4887019 | December 1989 | Reis et al. |
| 4887592 | December 1989 | Loertscher |
| 4891043 | January 1990 | Zeimer et al. |
| 4900143 | February 1990 | Bessler et al. |
| 4900145 | February 1990 | Akiyama |
| 4901718 | February 1990 | Bille |
| 4902124 | February 1990 | Roy, Sr. et al. |
| 4903695 | February 1990 | Warner et al. |
| 4905711 | March 1990 | Bennett et al. |
| 4907586 | March 1990 | Bille |
| 4911160 | March 1990 | Thyzel |
| 4911711 | March 1990 | Telfair et al. |
| 4917486 | April 1990 | Raven et al. |
| 4931053 | June 1990 | L'Esperance, Jr. |
| 4941093 | July 1990 | Marshall et al. |
| 4951663 | August 1990 | L'Esperance, Jr. |
| 4953969 | September 1990 | Fedorov |
| 4966577 | October 1990 | Crosson et al. |
| 4972836 | November 1990 | Schenck et al. |
| 4973330 | November 1990 | Azema et al. |
| 4976709 | December 1990 | Sand |
| 4988348 | January 1991 | Bille |
| 4994058 | February 1991 | Raven et al. |
| 5000561 | March 1991 | Lawniczak et al. |
| 5000751 | March 1991 | Schroder et al. |
| 5002571 | March 1991 | O'Donnell, Jr. et al. |
| 5013311 | May 1991 | Nouri |
| 5019074 | May 1991 | Muller |
| 5041134 | August 1991 | O'Donnell |
| 5048946 | September 1991 | Sklar et al. |
| 5049147 | September 1991 | Danon |
| 5054907 | October 1991 | Sklar et al. |
| 5057102 | October 1991 | Tomioka et al. |
| 5067951 | November 1991 | Greve |
| 5090798 | February 1992 | Kohayakawa |
| 5092863 | March 1992 | Schanzlin |
| 5098426 | March 1992 | Sklar |
| 5102409 | April 1992 | Balgorod |
| 5108388 | April 1992 | Trokel |
| 5108412 | April 1992 | Krumeich et al. |
| 5112328 | May 1992 | Taboada et al. |
| 5116114 | May 1992 | Nakamura et al. |
| 5122135 | June 1992 | Durr et al. |
| 5123902 | June 1992 | Muller et al. |
| 5128509 | July 1992 | Black et al. |
| 5133708 | July 1992 | Smith |
| 5137530 | August 1992 | Sand |
| 5141506 | August 1992 | York |
| 5147349 | September 1992 | Johnson et al. |
| 5147352 | September 1992 | Azema et al. |
| 5152055 | October 1992 | L'Esperance, III et al. |
| 5152759 | October 1992 | Parel et al. |
| 5163934 | November 1992 | Munnerlyn |
| 5171242 | December 1992 | Dewey et al. |
| 5174021 | December 1992 | L'Esperance, III et al. |
| 5178635 | January 1993 | Gwon et al. |
| 5188631 | February 1993 | L'Esperance, Jr. |
| 5194948 | March 1993 | L'Esperance, III et al. |
| 5196006 | March 1993 | Klopotek et al. |
| 5196027 | March 1993 | Thompson et al. |
| 5201730 | April 1993 | Easley et al. |
| 5203353 | April 1993 | Easley et al. |
| 5207668 | May 1993 | L'Esperance, Jr. |
| 5213092 | May 1993 | Uram |
| 5215104 | June 1993 | Steinert |
| 5217459 | June 1993 | Kamerling |
| 5219343 | June 1993 | L'Esperance, Jr. |
| 5219344 | June 1993 | Yoder, Jr. |
| 5222981 | June 1993 | Werblin |
| 5224942 | July 1993 | Beuchat et al. |
| 5226903 | July 1993 | Mizuno |
| 5246435 | September 1993 | Bille |
| 5246436 | September 1993 | Rowe |
| 5257988 | November 1993 | L'Esperance, Jr. |
| 5258025 | November 1993 | Fedorov et al. |
| 5263950 | November 1993 | L'Esperance, Jr. |
| 5263951 | November 1993 | Spears et al. |
| 5275593 | January 1994 | Easley et al. |
| 5277911 | January 1994 | Viegas et al. |
| 5279298 | January 1994 | Flower |
| 5279611 | January 1994 | McDonnell et al. |
| 5281211 | January 1994 | Parel et al. |
| 5282798 | February 1994 | Bruse et al. |
| 5284477 | February 1994 | Hanna et al. |
| 5288293 | February 1994 | O'Donnell, Jr. |
| 5290272 | March 1994 | Burstein et al. |
| 5295989 | March 1994 | Nakamura |
| 5300020 | April 1994 | L'Esperance, Jr. |
| 5300061 | April 1994 | Easley et al. |
| 5300062 | April 1994 | Ueno |
| 5300063 | April 1994 | Tano et al. |
| 5300114 | April 1994 | Gwon et al. |
| 5304168 | April 1994 | Sun |
| 5304169 | April 1994 | Sand |
| 5311224 | May 1994 | Enomoto |
| 5312320 | May 1994 | L'Esperance, Jr. |
| 5312393 | May 1994 | Mastel |
| 5314422 | May 1994 | Nizzola |
| 5318047 | June 1994 | Davenport et al. |
| 5318560 | June 1994 | Blount et al. |
| 5323788 | June 1994 | Silvestrini et al. |
| 5324281 | June 1994 | Muller |
| 5325134 | June 1994 | Kohayakawa |
| 5334190 | August 1994 | Seiler |
| 5336215 | August 1994 | Hsueh et al. |
| 5336216 | August 1994 | Dewey |
| 5342351 | August 1994 | Blaha et al. |
| 5342370 | August 1994 | Simon et al. |
| 5345948 | September 1994 | O'Donnell, Jr. |
| 5346491 | September 1994 | Oertli |
| 5347329 | September 1994 | Ota |
| 5348551 | September 1994 | Spears et al. |
| 5350374 | September 1994 | Smith |
| 5354331 | October 1994 | Schachar |
| 5355181 | October 1994 | Ashizaki |
| 5356407 | October 1994 | Easley et al. |
| 5356409 | October 1994 | Nizzola |
| 5360424 | November 1994 | Klopotek |
| 5364388 | November 1994 | Koziol |
| 5364390 | November 1994 | Taboada et al. |
| 5368590 | November 1994 | Itoh |
| 5370641 | December 1994 | O'Donnell, Jr. |
| 5372595 | December 1994 | Gaasterland et al. |
| 5374265 | December 1994 | Sand |
| 5376086 | December 1994 | Khoobehi et al. |
| 5391165 | February 1995 | Fountain et al. |
| 5395356 | March 1995 | King et al. |
| 5403307 | April 1995 | Zelman |
| 5408484 | April 1995 | Weimel |
| 5411501 | May 1995 | Klopotek |
| 5412561 | May 1995 | Rosenshein et al. |
| 5413555 | May 1995 | McMahan |
| 5423798 | June 1995 | Crow |
| 5423800 | June 1995 | Ren et al. |
| 5423801 | June 1995 | Marshall et al. |
| 5425727 | June 1995 | Koziol |
| 5425729 | June 1995 | Ishida et al. |
| 5425730 | June 1995 | Luloh |
| 5437657 | August 1995 | Epstein |
| 5437658 | August 1995 | Muller et al. |
| 5439462 | August 1995 | Bille |
| 5441496 | August 1995 | Easley et al. |
| 5441511 | August 1995 | Hanna |
| 5442412 | August 1995 | Frey et al. |
| 5442487 | August 1995 | Mizuno |
| 5445633 | August 1995 | Nakamura et al. |
| 5460627 | October 1995 | O'Donnell, Jr. |
| 5461212 | October 1995 | Seiler et al. |
| 5462739 | October 1995 | Dan et al. |
| 5465737 | November 1995 | Schachar |
| 5470329 | November 1995 | Sumiya |
| 5474548 | December 1995 | Knopp et al. |
| 5476511 | December 1995 | Gwon et al. |
| 5480396 | January 1996 | Simon |
| 5484432 | January 1996 | Sand |
| 5489299 | February 1996 | Schachar |
| 5503165 | April 1996 | Schachar |
| 5507740 | April 1996 | O'Donnell, Jr. |
| 5514124 | May 1996 | Alpins |
| 5514125 | May 1996 | Lasser et al. |
| 5520679 | May 1996 | Lin |
| 5527774 | June 1996 | Girard |
| 5529076 | June 1996 | Schachar |
| 5533997 | July 1996 | Ruiz |
| 5548352 | August 1996 | Dewey |
| 5549597 | August 1996 | Shimmick et al. |
| 5556395 | September 1996 | Shimmick et al. |
| 5573544 | November 1996 | Simon et al. |
| 5594753 | January 1997 | Frey et al. |
| 5616139 | April 1997 | Okamoto |
| 5618284 | April 1997 | Sand |
| 5620435 | April 1997 | Belkin |
| 5627162 | May 1997 | Gwon et al. |
| 5632742 | May 1997 | Frey et al. |
| 5651782 | July 1997 | Simon et al. |
| 5656186 | August 1997 | Mourou et al. |
| 5684560 | November 1997 | Roffman et al. |
| 5697945 | December 1997 | Kritzinger |
| 5709868 | January 1998 | Perricone |
| 5722952 | March 1998 | Schachar |
| 5731909 | March 1998 | Schachar |
| 5772970 | March 1998 | Colvard et al. |
| 5738677 | April 1998 | Colvard et al. |
| 5752950 | May 1998 | Frey et al. |
| 5773472 | June 1998 | Stjernschantz et al. |
| 5828686 | October 1998 | Frey et al. |
| 5843184 | December 1998 | Cionni |
| 5849006 | December 1998 | Frey et al. |
| 5886768 | March 1999 | Knopp et al. |
| 5907908 | June 1999 | Cunanan et al. |
| 5912915 | June 1999 | Reed et al. |
| 5919186 | July 1999 | Bath |
| 5980513 | November 1999 | Frey et al. |
| 5984916 | November 1999 | Lai |
| 5993441 | November 1999 | Muller et al. |
| 6004314 | December 1999 | Wei |
| 6007578 | December 1999 | Schachar |
| 6013101 | January 2000 | Israel |
| 6019472 | February 2000 | Koester et al. |
| 6027494 | February 2000 | Frey |
| 6050687 | April 2000 | Bile et al. |
| 6055259 | April 2000 | Frey et al. |
| 6059772 | May 2000 | Hsia et al. |
| 6070981 | June 2000 | Mihashi et al. |
| 6099522 | August 2000 | Knopp |
| 6132424 | October 2000 | Tang |
| 6186148 | February 2001 | Okada |
| 6190375 | February 2001 | Frey |
| 6197018 | March 2001 | O'Donnell |
| 6197056 | March 2001 | Schachar |
| 6252595 | June 2001 | Birmingham et al. |
| 6312422 | June 2001 | Dubnack |
| 6254595 | July 2001 | Juhasz et al. |
| 6261220 | July 2001 | Frey et al. |
| 6271914 | August 2001 | Frey et al. |
| 6271915 | August 2001 | Frey et al. |
| 6275718 | August 2001 | Lempert |
| 6280435 | August 2001 | Odrich et al. |
| 6280468 | August 2001 | Schachar |
| 6299640 | October 2001 | Schachar |
| 6302879 | October 2001 | Frey et al. |
| 6312424 | November 2001 | Largent |
| 6313165 | November 2001 | Grunberger et al. |
| 6315773 | November 2001 | Frey et al. |
| 6319274 | November 2001 | Shadduck |
| 6322545 | November 2001 | Schachar |
| 6322554 | November 2001 | Tomita |
| 6322556 | November 2001 | Gwon |
| 6324191 | November 2001 | Horvath |
| 6325791 | December 2001 | Shimoji |
| 6325792 | December 2001 | Swinger et al. |
| 6328732 | December 2001 | Donitzky et al. |
| 6344040 | February 2002 | Juhasz et al. |
| 6373571 | April 2002 | Juhasz et al. |
| D459806 | July 2002 | Webb |
| D459807 | July 2002 | Webb |
| 6413262 | July 2002 | Saishin et al. |
| D462442 | September 2002 | Webb |
| D462443 | September 2002 | Webb |
| 6451008 | September 2002 | Frey et al. |
| 6460997 | October 2002 | Frey et al. |
| 6467906 | October 2002 | Alpins |
| 6493151 | December 2002 | Schachar |
| 6494910 | December 2002 | Ganem et al. |
| 6497483 | December 2002 | Frey et al. |
| 6530917 | March 2003 | Seiler et al. |
| 6544254 | April 2003 | Bath |
| 6547394 | April 2003 | Doherty |
| 6554825 | April 2003 | Murray et al. |
| 6585726 | July 2003 | Frey et al. |
| 6588902 | July 2003 | Isogai |
| 6623476 | September 2003 | Juhasz et al. |
| 6626893 | September 2003 | Frey et al. |
| 6626894 | September 2003 | Frey et al. |
| 6626895 | September 2003 | Frey et al. |
| 6626896 | September 2003 | Frey et al. |
| 6626897 | September 2003 | Frey et al. |
| 6626898 | September 2003 | Frey et al. |
| 6648877 | November 2003 | Juhasz et al. |
| 6669342 | December 2003 | Lieberman et al. |
| 6676653 | January 2004 | Juhasz et al. |
| 6693927 | February 2004 | Horvath et al. |
| 6702853 | March 2004 | Peyman |
| 6726679 | April 2004 | Dick et al. |
| 6863667 | March 2005 | Webb et al. |
| 6905641 | June 2005 | Platt et al. |
| 6923955 | August 2005 | Till et al. |
| 6962583 | November 2005 | Kadziauskas et al. |
| 7077838 | July 2006 | Wong |
| 7182759 | February 2007 | Kadziauskas et al. |
| 7220255 | May 2007 | Lai |
| 7252662 | August 2007 | McArdle et al. |
| RE40002 | January 2008 | Lin |
| RE40184 | March 2008 | Lin |
| 7338167 | March 2008 | Zelvin et al. |
| 7357504 | April 2008 | Fischer et al. |
| 7364575 | April 2008 | Van Saarloos |
| 7390089 | June 2008 | Loesel et al. |
| RE40420 | July 2008 | Dick et al. |
| 7402159 | July 2008 | Loesel et al. |
| 7540613 | June 2009 | Severns |
| 7655002 | February 2010 | Myers |
| 7717908 | May 2010 | Ruiz et al. |
| 7766903 | August 2010 | Blumenkranz et al. |
| 7836894 | November 2010 | Brinkmann et al. |
| 8262646 | September 2012 | Frey |
| 8382745 | February 2013 | Naranjo-Tackman |
| 8394084 | March 2013 | Palankar et al. |
| 8403921 | March 2013 | Palankar et al. |
| 8425497 | April 2013 | Blumenkranz et al. |
| 8465478 | June 2013 | Frey |
| 8480659 | July 2013 | Frey |
| 8500723 | August 2013 | Frey |
| 8617146 | December 2013 | Frey |
| 8758332 | June 2014 | Frey |
| 8801186 | August 2014 | Frey |
| 9180051 | November 2015 | Frey |
| 9375349 | June 2016 | Frey |
| 9545338 | January 2017 | Frey |
| 2001/0010003 | July 2001 | Lai |
| 2001/0029363 | October 2001 | Um |
| 2002/0004658 | January 2002 | Munnerlyn |
| 2002/0025311 | February 2002 | Till |
| 2002/0029053 | March 2002 | Gordon |
| 2002/0049450 | April 2002 | Myers |
| 2002/0103478 | August 2002 | Gwon et al. |
| 2002/0103481 | August 2002 | Webb |
| 2002/0110549 | August 2002 | Till |
| 2002/0138139 | September 2002 | Till |
| 2002/0140903 | October 2002 | Schachar |
| 2003/0050629 | March 2003 | Kadziauskas |
| 2003/0055412 | March 2003 | Lieberman |
| 2003/0109926 | June 2003 | Portney |
| 2003/0135272 | July 2003 | Brady et al. |
| 2003/0139737 | July 2003 | Lin |
| 2003/0212387 | November 2003 | Kurtz et al. |
| 2003/0220630 | November 2003 | Lin |
| 2004/0054359 | March 2004 | Ruiz |
| 2004/0059321 | March 2004 | Knopp et al. |
| 2004/0070761 | April 2004 | Horvath et al. |
| 2004/0143244 | July 2004 | Gray et al. |
| 2004/0199149 | October 2004 | Myers |
| 2004/0199150 | October 2004 | Lai |
| 2004/0243111 | December 2004 | Bendett |
| 2004/0249403 | December 2004 | Loomas et al. |
| 2005/0107775 | May 2005 | Huang et al. |
| 2005/0165387 | July 2005 | Lubatschowski et al. |
| 2005/0197655 | September 2005 | Telfair et al. |
| 2005/0203492 | September 2005 | Nguyen |
| 2005/0243276 | November 2005 | Van Heugten et al. |
| 2006/0058682 | March 2006 | Miller et al. |
| 2006/0192921 | August 2006 | Loesel et al. |
| 2006/0195076 | August 2006 | Blumenkranz et al. |
| 2006/0215111 | September 2006 | Mihashi |
| 2006/0259022 | November 2006 | Lin |
| 2007/0010803 | January 2007 | Bischoff |
| 2007/0078447 | April 2007 | Weinacht et al. |
| 2007/0093795 | April 2007 | Melcher et al. |
| 2007/0093796 | April 2007 | Raksi et al. |
| 2007/0129693 | June 2007 | Hunter et al. |
| 2007/0173794 | July 2007 | Frey |
| 2007/0185475 | August 2007 | Frey et al. |
| 2007/0265603 | November 2007 | Pinelli |
| 2008/0071254 | March 2008 | Lummis et al. |
| 2008/0111972 | May 2008 | Barth et al. |
| 2008/0281303 | November 2008 | Culbertson et al. |
| 2008/0281413 | November 2008 | Culbertson et al. |
| 2008/0287928 | November 2008 | Arnoldussen |
| 2008/0312675 | December 2008 | Newcott et al. |
| 2009/0069794 | March 2009 | Kurtz |
| 2009/0088734 | April 2009 | Mordaunt |
| 2009/0126870 | May 2009 | Zadoyan et al. |
| 2009/0131921 | May 2009 | Kurtz et al. |
| 2009/0137988 | May 2009 | Kurtz |
| 2009/0137991 | May 2009 | Kurtz |
| 2009/0137993 | May 2009 | Kurtz |
| 2009/0157063 | June 2009 | Ruiz et al. |
| 2009/0161065 | June 2009 | Smith, III et al. |
| 2009/0171327 | July 2009 | Kurtz et al. |
| 2009/0177189 | July 2009 | Raksi |
| 2009/0244482 | October 2009 | Elsner et al. |
| 2009/0281530 | November 2009 | Korn |
| 2010/0002837 | January 2010 | Gertner et al. |
| 2010/0004641 | January 2010 | Frey |
| 2010/0004643 | January 2010 | Frey et al. |
| 2010/0022994 | January 2010 | Frey et al. |
| 2010/0022995 | January 2010 | Frey et al. |
| 2010/0022996 | January 2010 | Frey et al. |
| 2010/0042079 | February 2010 | Frey et al. |
| 2010/0060855 | March 2010 | Graether |
| 2010/0114079 | May 2010 | Myers et al. |
| 2010/0256614 | October 2010 | Donitzky et al. |
| 2010/0256615 | October 2010 | Blumenkranz et al. |
| 2010/0292676 | November 2010 | Larsen |
| 2010/0292678 | November 2010 | Frey et al. |
| 2010/0312231 | December 2010 | Singh |
| 2010/0324542 | December 2010 | Kurtz |
| 2011/0022035 | January 2011 | Porter et al. |
| 2011/0022036 | January 2011 | Frey et al. |
| 2011/0028950 | February 2011 | Raksi et al. |
| 2011/0092965 | April 2011 | Slatkine et al. |
| 2011/0118712 | May 2011 | Lubatschowski et al. |
| 2011/0137301 | June 2011 | Bartoli |
| 2011/0149240 | June 2011 | Alpins |
| 2011/0160710 | June 2011 | Frey et al. |
| 2011/0160711 | June 2011 | Naranjo-Tackman et al. |
| 2011/0166557 | July 2011 | Naranjo-Tackman et al. |
| 2011/0184395 | July 2011 | Schuele et al. |
| 2011/0187995 | August 2011 | Frey et al. |
| 2011/0190739 | August 2011 | Frey et al. |
| 2011/0190740 | August 2011 | Frey et al. |
| 2011/0292340 | December 2011 | Shimizu et al. |
| 2012/0182522 | July 2012 | Frey et al. |
| 2553963 | Aug 2005 | CA | |||
| 2680072 | Sep 2008 | CA | |||
| 0 397 962 | Nov 1990 | EP | |||
| 2 497 087 | Jul 1982 | FR | |||
| 5-115437 | May 1993 | JP | |||
| WO 1991-19539 | Dec 1991 | WO | |||
| WO 01/13838 | Mar 2001 | WO | |||
| WO 2005/039462 | May 2005 | WO | |||
| WO-2005039462 | May 2005 | WO | |||
| WO 2005/070358 | Aug 2005 | WO | |||
Other References
|
Al-Ghoul, K. J. et al., "Distribution and Type of Morphological Damage in Human Nuclear Age-Related Cataracts", Department of Cell Biology and Anatomy, University of North Carolina and Duke University Eye Center, 1996, pp. 237-251. cited by applicant . Anschutz, Till, M.D., "Laser Correction of Hyperopia and Presbyopia", Int Ophtalmol Clin, 1994, vol. 34, No. 4, pp. 107-137. cited by applicant . Armstrong, Larry "A cataract Breakthrough May Be on the Way", Business Week, Mar. 23, 1998, pp. 90-92. cited by applicant . Aston, Adam, "Why Settle for 20/20?", Business Week, Mar. 17, 2003, pp. 95-96. cited by applicant . Back, Arthur P. et al., "Correction of Presbyopia with Contact Lenses: Comparative Success Rates with Three Systems", Optometry & Vision Science, 1989, vol. 66, No. 8, pp. 518-525. cited by applicant . Bath, Patricia E. et al., "Endocapsular Excimer Laser Phakoablation Through a 1-mm Incision", Opthalmic Laser Therapy, 1987, vol. 2, No. 4, pp. 245-248. cited by applicant . Beers, A. P. A. et al. "Age-Related Changes in the Accommodation Mechanism", Optometry and Vision Science, 1996, vol. 73, No. 4, pp. 235-242. cited by applicant . Beers, A. P. A. et al., "In Vivo Determination of the Biomechanical Properties of the Component Elements of the Accommodation Mechanism", Vision Res., 1994, vol. 34, pp. 2897-2905. cited by applicant . Bellows, John G., M.D. et al., "B. Cataracta Complicata". cited by applicant . Bor, Zs. PhD., et al., "Plume Emission, Shock Wave and Surface Wave Formation During Excimer Laser Ablation of the Cornea", Supplement to Retroactive & Corneal Surgery, vol. 9, Mar./Apr. 1993, pp. S110-S115. cited by applicant . Borkman, Raymond F. "Evidence for a Free Radical Mechanism in Aging and u.v.-Irradiated Ocular Lenses", Exp. Eye Res., 1977, vol. 25, pp. 303-309. cited by applicant . Braham, Lewis, "Eye Surgery: It's Getting Sharper", Business Week, Oct. 18, 2004, pp. 142-143. cited by applicant . Bron, A.J., "The Ageing Lens", Opthalmologica, 2000, vol. 214, pp. 86-104. cited by applicant . Brown, Nicholas, "Dating the onset of cataract", Trans. Opthal. Soc. U.K., 1976, vol. 96, pp. 18-23. cited by applicant . Brown, Nicholas "The Change in Lens Curvature with Age", Exp. Eye Res., 1974, vol. 19, pp. 175-183. cited by applicant . Brown, Nicholas "The Change in Shape and Internal Form of the Lens of the Eye on Accommodation", Exp. Eye Res., 1973, vol. 15, pp. 441-459. cited by applicant . Campbell, Melanie C. W., "Measurement of Refractive Index in an Intact Crystalline Lens", Vision Res., 1984, vol. 24, No. 5, pp. 409-415. cited by applicant . Charles, M. W. et al., "Dimensions of the Human Eye Relevant to Radiation Protection", Phys. Med. Biol., 1975, vol. 20, No. 2, pp. 202-218. cited by applicant . Cook, Christopher A. et al., "Aging of the Human Crystalline Lens and Anterior Segment", Vision Res., 1994, vol. 34, No. 22, pp. 2945-2954. cited by applicant . Costagliola, Ciro et al., "ArF 193 nm Excimer Laser Corneal Surgery as a Possible Risk Factor in Cataractogenesis", Exp. Eye Res., 1994, vol. 58, pp. 453-457. cited by applicant . Cotlier, Edward, M.D., "The Lens", Adler's Physiology of the Eye, 1994 pp. 268-290. cited by applicant . Cromie, William J., "Laser Makes History's Fastest Holes", The Harvard University Gazette, Obtained from the Internet on Nov. 22, 1999 at: http://www.news.harvard.edu/gazette/1999/10.07/laser.html, 6 pages. cited by applicant . Fagerholm, P.P., "The Response of the Lens to Trauma", Trans. Ophtal. Soc. U. K., 1982, vol. 102, pp. 369-374. cited by applicant . Farxsworth, P.N. et al., "Anterior Zonular Shifts with Age", Exp. Eye Res., 1979, vol. 28, pp. 291-297. cited by applicant . Fisher, R. F. et al., "The elastic constants and ultrastructural organization of a basement membrane (lens capsule)", Proc. R. Soc. Lond. B., 1976, vol. 193, pp. 335-358. cited by applicant . Fisher, R. F., "The Mechanics of Accommodation in Relation to Presbyopia", Eye, 1988, vol. 2, pp. 646-649. cited by applicant . Fisher, R. F., "The Ciliary Body in Accommodation", Trans. Opthalmol. Soc. U.K., 1986, vol. 105, pp. 208-219. cited by applicant . Fisher, R.F., "Elastic Constants of the Human Lens Capsule", J. Physiol., 1969, vol. 201, pp. 1-19. cited by applicant . Fleck, Brian W. et al., "Q-switched Nd:YAG laser disruption of rabbit lens nucleus", Laser and Light in Ophthalmology, 1990, vol. 3. No. 3, pp. 227-232. cited by applicant . Garner, Margaret H. et al., "Selective oxidation of cysteine and methionine in normal and senile cataractous lenses", Proc. Natl. Acad. Sci. USA, 1980, vol. 77, No. 3, pp. 1274-1277. cited by applicant . Giblin, Frank J. et al., "Nuclear Light Scattering, Disulfide Formation and Membrane Damage in Lenses of Older Guinea Pigs Treated with Hyperbaric Oxygen", Exp. Eye Res., 1995, vol. 60, pp. 219-235. cited by applicant . Gimbel, Howard V. et al., "Intrastromal Photorefractive Keratectomy with the Nd:YLF Laser", Int. Ophthalmol Ciln., 1994 vol. 34, No. 4, pp. 139-145. cited by applicant . Goodenough, Daniel A., "Lens gap junctions: a structural hypothesis for nonregulated low-resistance intercellular pathways", Invest. Ophthalmol. Visual Sci., 1979, vol. 18, No. 11, pp. 1104-1122. cited by applicant . Habib, Maged S. et al., "Myopic Intrastromal Photorefractive Keratectomy With the Neodymium-Yttrium Lithium Fluoride Picosecond Laser in the Cat Cornea", Arch Ophthalmol., 1995, vol. 113, pp. 499-505. cited by applicant . Hahn, D.W., "Dynamics of Ablation Plume Particles Generated During Excimer Laser Corneal Ablation", Lasers in Surgey and Medicine, 1995, vol. 16, pp. 384-389. cited by applicant . Hara, Tsutomu, M.D. et al., "Complications associated with endocapsular balloon implantation rabbit eyes", J Cataract Refract Surg, 1994, vol. 20, pp. 507-508. cited by applicant . Harding, J. J., "Disulphide Cross-linked Protein of High Molecular Weight in Human Cataractous Lens", Exp. Eye Res., 1973, vol. 17, pp. 377-383. cited by applicant . Hemenger, Richard P. et al., "Change With Age of the Refractive Index Gradient of the Human Ocular Lens", Investigative Ophthalmology & Visual Science, 1995. vol. 36, No. 3, pp. 703-707. cited by applicant . Horwitz, Joseph, ".alpha.-Crystallin can function as a molecular chaperone", Proc. Natl. Acad. Sci. USA, 1992, vol. 89. pp. 10449-10453. cited by applicant . Hu, Tian-Sheng et al., "Reversal of Galactose Cataract with Sorbinil in Rats", Investigative Ophthalmology & Visual Science, May 1983, vol. 24, pp. 640-644. cited by applicant . Jacques, Paul F. et al., "Long-term vitamin C supplement use and prevalence of early age-related lens opacities", Am J Clin Nutr, 1997, vol. 6, pp. 911-916. cited by applicant . Juhasz, Tibor, Ph.D. et al., "Dynamics of Shock Waves and Cavitation Bubbles Generated by Picosecond Laser Pulses in Corneal Tissue and Water", Lasers in Surgery and Medicine, 1994, vol. 15, pp. 91-98. cited by applicant . Kaufman, Paul L., M.D., "Accommodation and Presbyopia: Neuromuscular and Biophysical Aspects", Adler's Physiology of the Eye, 1994, pp. 391-411. cited by applicant . Keeney, Arthur H., M.D., "Intralenticular Foreign Bodies", Arch Ophthal., 1971, vol. 86, pp. 499-501. cited by applicant . Koretz, Jane F. et al., "The Zones of Discontinuity in the Human Lens: Development and Distribution with Age", Vision Res., 1994, vol. 34, No. 22, pp. 2955-2962. cited by applicant . Koretz, Jane F. et al., "Analysis of Human Crystalline Lens Curvature as a Function of Accommodative State and Age", Vision Res., 1984, vol. 24, No. 10, pp. 1141-1151. cited by applicant . Koretz, Jane F. et al., "Model of the Accommodative Mechanism in the Human Eye", Vis. Res., 1982, vol. 22, pp. 917-927. cited by applicant . Koretz, Jane F. et al., "How the Human Eye Focuses", Scientific American, 1988, pp. 92-99. cited by applicant . Koretz, Jane F. et al., "A Model for Accommodation in the Young Human Eye: The Effects of Lens Elastic Anisotropy on the Mechanism", Vision Res., 1983, vol. 23, No. 12, pp. 1679-1686. cited by applicant . Koretz, Jane F. et al., "Accommodation and Presbyopia in the Human Eye--Aging of the Anterior Segment", Vision Res., 1989, vol. 29, No. 12, pp. 1685-1692. cited by applicant . Krag, Susanne et al., "Biomechanical Characteristics of the Human Anterior Lens Capsule in Relation to Age", Investigative Ophthalmology & Visual Science, 1997, vol. 58, No. 2, pp. 357-362. cited by applicant . Kronemyer, Bob, "Accommodating IOL? Impossible, Recent Study Seems to Say". Ocular Surgery News, 1996, obtained from the Internet at: http://www.slackmc.com, on May 13, 1997. cited by applicant . Krueger, Ronald R., M.D., et al., "Nonmechanical Microkeratomes Using Laser and Water Jet Technology". cited by applicant . Krueger, Ronald R., M.D. et al., "Ultrastructure of Picosecond Laser Intrastromal Photodisruption", Journal of Retractive Surgery, 1996, vol. 12, pp. 607-612. cited by applicant . Kurtz, Ron M., MD, et al., "Photodisruption in the Human Cornea as a Function of Laser Pulse Width", Journal of Refractive Surgery, 1997, vol. 13, pp. 653-658. cited by applicant . Kuszak, J. R. et al., "Biochemistry of the Crystalline Lens; Anatomy of Aged and Senile Cataractous Lenses", pp. 564-575. cited by applicant . Kuszak, J. R. et al., "Lens Optical Quality and Lens Sutures", Investigative Ophthalmology & Visual Science, 1991, vol. 32, No. 7, pp. 2123-2129. cited by applicant . Kuszak, J. R. et al., "Lens Optical Quality is a Direct Function of Lens Sutural Architecture", Investigative Ophthalmology & Visual Science, 1991, vol. 32, No. 7, pp. 2119-2122. cited by applicant . Kuszak, J. et al., "The Surface Morphology of Embryonic and Adult Chick Lens-Fiber Cells", The American Journal of Anatomy, 1960, pp. 395-410. cited by applicant . Kuszak, J. et al., "Gap Junctions of Chick Lens Fiber Cells", Exp. Eye Res. 27, 1978, pp. 495-498. cited by applicant . Kuwabara, Toichiro, et al., "Electron Microscopic Study of Galactose-Induced Cataract", Investigative Ophthalmology, 1969, vol. 8, No. 2, pp. 133-149. cited by applicant . Lerman, Sidney, et al., "A Method for Detecting 8-Methoxypsoralen in the Ocular Lens", Science, 1977, vol. 197, 1287-1288. cited by applicant . Lerman, Sidney, et al., "Spectroscopic Evaluation and Classification of the Normal, Aging, and Cataractous Lens", Opthl. Res., 8, 1976, pp. 335-353. cited by applicant . Lerman, Sidney, et al., "Photosensitization of the lens by 8-meth-oxypsoralen", Invent. Ophthalmol. Visual Sci., 1977, vol. 16, No. 11, pp. 1066-1068. cited by applicant . Lerman, Sidney, et al., "Psoralen-long-wave Ultraviolet Therapy and Human Cataractogenesis", Invent. Ophthalmol. Visual Sci., 1982, vol. 23, No. 6, pp. 801-804. cited by applicant . Lerman, Sidney, M.D., "Photosensitizing Drugs and Their Possible Role in Enhancing Ocular Toxicity", Ophthalmology, 1986, vol. 93, No. 3, pp. 304-318. cited by applicant . Lim, Seung Jeong, M.D. et al., "Analysis of zonular-free zone and lens size in relation to axial length of eye with age", J Cataract Refract Surg, 1998, vol. 24, pp. 390-396. cited by applicant . Lou, Marjorie F., et al., Protein-Thiol Mixed Disulfides in Human Lens, Academic Press Limited, 1992, pp. 889-896. cited by applicant . Lutze, Margaret et al., "Lenses of Diabetic Patients "Yellow" at an Accelerated Rate Similar to Older Normals", Investigative Opholamology & Visual Science, 1991, vol. 32, No. 1, pp. 194-199. cited by applicant . Maguen, Ezra, et al., "Excimer Laser Ablation of the Human Lens at 308 nm with a Fiber Delivery System", J. Cataract Refract Surg., 1989, vol. 15, pp. 409-414. cited by applicant . McDonald, Marguerita B., et al., "Central Photorefractive Keratectomy for Myopia", Arch Ophthalmol, 1990, vol. 108, pp. 799-808. cited by applicant . Mutri, Donald O., et al., "A Video Technique for Phakometry of the Human Crystalline Lens", Investigative Opthalmology, & Visual Science, 1992, vol. 33, No. 5, pp. 1771-1781. cited by applicant . Nanevicz, Tania M., et al., "Excimer Laser Ablation of the Lens", Arch Opthalmol, 1986, vol. 104, pp. 1825-1829. cited by applicant . O'Donnell, Colleen B., et al., "Ablation Smoothness as a Function of Excimer Laser Delivery System", J. Cataract Refract Surg., 1996, vol. 22, pp. 682-685. cited by applicant . O'Donnell, Colleen B., et al., "Surface Roughness in PMMA is Linearly Related to the Amount of Excimer Laser Ablation", Journal of Refractive Surgery, 1996, vol. 12, pp. 171-174. cited by applicant . Pau, Hans et al., "The increasing sclerosis of the human lens with age and its relevance to accommodation and presbyopia", Graefe's Arch Clin Exp. Ophthalmol, 1991, vol. 229, pp. 294-296. cited by applicant . Puliafito, Carmen A., M.D. et al., "High-Speed Photography of Excimer Laser Ablatio of the Cornea", Arch Ophthalmol, 1987, vol. 105, pp. 1255-1259. cited by applicant . Rafferty, Nancy et al., "Lens Wound Healing and Cataractogenesis in a Pigmented Eye", Exp. Eye Res., 1984, vol. 38, pp. 267-277. cited by applicant . Riley, Michael V., et al., "The Effects of UV-B Irradiation on the Corneal Endothelium", Eye Research Institute of Okland Universityl, 1987, pp. 1021-1033. cited by applicant . Schachar, Ronald A., M.D., "Cause and Treatment of Presbyopia With a Method for Increasing the Amplitude of Accommodation", Annals of Ophthalmol, 1992, vol. 24, pp. 445-452. cited by applicant . Schachar, Ronald A., M.D. et al., "Experimental Support for Schachar's Hypothesis of Accommodation", Ann Ophthalmol, 1993, vol. 25, pp. 404-409. cited by applicant . Schachar, Ronald A., M.D. et al., "Experimental Destruction of Cataractous Lenses by Laser", Ophthalmic Surgery, Surgical Forum, pp. 506-509. cited by applicant . Schachar, Ronald A. MD, PhD., et al., "A Revolutionary Variable Focus Lens", Annals of Ophthalmology, 1996, vol. 28, No. 1, pp. 11-18. cited by applicant . Schachar, Ronald A., MD, PhD, "Histology of the Ciliary Muscle-Zonular Conections", Annals of Opthalmology, 1996, vol. 28, No. 2, pp. 70-79. cited by applicant . Schachar, Ronald A., MD, PhD, "Pathophysiology of Accommodation and Presbyopia, Understanding the Clinical Implications", J. Florida M.A., 1994, vol. 81, No. 4, pp. 268-271. cited by applicant . Spector, Abraham, "Aging of the Lens and Cataract Formation", Aging and Human Visual Function, 1982 pp. 27-43. cited by applicant . Srinivasan, R., "Ablation of Polymers and Biological Tissue by Ultraviolet Lasers", Oct. 1986, pp. 559-565. cited by applicant . Swegmark, Gunnar, "Studies With Impedance Cyclography on Human Ocular Accommodation at Different Ages", ACTA Opthalmologica, 1969, vol. 47, pp. 1186-1206. cited by applicant . Taboada, J., et al., "Optically Coupled Technique for Photorefractive Surgery of the Cornea", Optics Letters, 1990, vol. 15, No. 9, pp. 458-460. cited by applicant . Tamm, Svenja, et al., "Age-Related Changes of the Human Ciliary Muscle. A Quantitative Morphometric Study", Mechanisms of Aging and Development, 1992, vol. 62, pp. 209-221. cited by applicant . Taylor, Virginia L. et al., "Morphology of the Normal Human Lens", Investigative Ophthalmology & Visual Science, 1996, vol. 37, No. 7, pp. 1396-1410. cited by applicant . Topilow, Harvey W., M.D., "Vitreous Changes in Retinal Branch Vein Occlusion", Arch Ophthalmol, 1987, vol. 105, pp. 1165-165. cited by applicant . Trokel, Stephen L., M.D., et al., "Eximer Laser Surgery of the Cornea", American Journal of Opthalmology, 1983, vol. 96, No. 6, pp. 710-715. cited by applicant . Tsubota, Kazuo, "Application of Erbium: YAG Laser in Ocular Ablation", Ophthalmologica, 1990, vol. 200,pp. 117-122. cited by applicant . Van Alphen, G.W.H.M., et al., "Elasticity of Tissues Involved in Accommodation", Vision Res., 1991, vol. 31, No. 7/8, pp. 1417-1438. cited by applicant . Venugopalan, V., et al., "The Thermodynamic Response of Soft Biological Tissues to Ultraviolet Laser Irradiation", Biophysical Journal, 1995, vol. 60, pp. 1258-1271. cited by applicant . Vogel, Alfred, PhD., et al., "Factors Determining the Refractive Effects of Intrastromal Photorefractive Keratectomy with the Picosecond Laser", J. Cataract Refract Surg., 1997, vol. 23, pp. 1301-1310. cited by applicant . Vrensen, G. F. J. M., "Aging of the human eye lens--A morphological point of view", Comp. Biochem. Physiol., 1995, vol. 111A, pp. 519-532. cited by applicant . Waring III, George O., M.D., "Presbyopia and Accommodative Intraocular Lenses--the Next Frontier in Refractive Surgery?", Refractive & Corneal Surgery, 1992, vol. 8, pp. 421-423. cited by applicant . Weale, Robert D., SC., "Presbyopia Toward the End of the 20th Century", Survey of Opthalmology, 1989, vol. 34, No. 1,pp. 15-29. cited by applicant . Werblin, Theodore P., M.D., "Should We Consider Clear Lens Extraction for Routine Refractive Surgery?", Refractive & Corneal Surgery, 1992, vol. 8, pp. 480-481. cited by applicant . Wyatt, Harry J., "Application of a Simple Mechanical Model of Accommodation to the Aging Eye", Eye Res., 1993, vol. 33, No. 5/6, pp. 731-738. cited by applicant . Zuclich, Joseph A. et al., "In Situ Measurements of Lens Fluorescence and its Interference With Visual Function", Investigative Ophthalmology & Visual Science, 1993, vol. 33, No. 2, pp. 410-415. cited by applicant . Zuclich, Joseph A. et al., "A comparison of laser-induced retinal damage from infrared wavelengths to that from visible wavelengths", Lasers and Light, 1997, vol. 8, No. 1, pp. 15-29. cited by applicant . Zuclich, Joseph, "In Vivo Measurements of Optical Properties of the Ocular Lens", Reprinted from Proceedings of Ultraviolet Radiation Hazards, Jan. 26-27, 1994, SPIE-Ultraviolrt Radiation Hazards, 1994, vol. 2134B, pp. 99-112. cited by applicant . Zuclich, J.A., et al., "Ocular Effects of Penetrating IR Laser Wavelengths", Reprinted from Proceedings of Laser-Tissue Interaction VI, Feb. 6-9, 1995, SPIE--The International Society for Optical Engineering, 1995, vol. 2391, pp. 111-125. cited by applicant . Zuclich, Joseph A., et al., "Rapid Noninvasive Optical Characterization of the Human Lens", Lasers in the Life Sciences, 1994, vol. 6, No. 1, pp. 39-53. cited by applicant . Zuclich, Joseph A., "Workshop on Long-Term Visual Health Risks of Optical Radiation--Thermal Cataracts Induced by UV Laser Radiation", Workshop Report, Cataract Working Group, 13 pgs. cited by applicant . Zuclich, Joseph A., "Ultraviolet-Induced Photochemical Damage in Ocular Tissues", Health Physics, 1989, vol. 56, No. 5, pp. 671-681. cited by applicant . Zuclich, Joseph A., "Research on the Ocular Effects of Laser Radiation", Technology Incorporated: Life Sciences Division, Chapters 6-1 to 10-9. cited by applicant . Optical Radiation and Visual Health, pp. 28-33. cited by applicant . Rao, Ch. Mohan, et al., "Level of Reduced Nucleotides and Lens Photodamage", National Eye Institute, Bethesda, MD., 1 pg. cited by applicant . International Search Report dated Oct, 23, 2007 from related PCT application No. PCT/US07/01312, 1 page. cited by applicant . International Search Report dated Jan. 2, 2008 from related PCT application No. PCT/US07/01353, 1 page. cited by applicant . Akchurin, Garif et al., "Evaluation of the degree of turbidity if cataract lens and its correlation with retinal visual acuity", SPIE, vol. 3591, 1999, pp. 74-81. cited by applicant . Al-Ghoul, Kristin J. et al., "Structural Evidence of Human Nuclear Fiber Compaction as a Function of Ageing and Cataractogenesis", Exp. Eye Res., vol. 72, 2001, pp. 199-214. cited by applicant . Alio, et al., "Crystalline Lens Optical Dysfunction through Aging", Ophthalmology, vol. 112, No. 11, Nov. 2005, pp. 2022-2029. cited by applicant . Amann, Josef et al., "Increased Endothelial Cell Density in the Paracentral and Peripheral Regions of the Human Cornea", American Journal of Ophthalmology, vol. 135, No. 5, 2003, pp. 584-590. cited by applicant . Amendt, M. Strauss et al., "Modeling of bubble dynamics in relation to medical applications", SPIE, vol. 2975, 1997, pp. 362-373. cited by applicant . Ansari, Rafat R. et al., "Measuring lens opacity: combining quasi-elastic light scattering with Scheimpflug imaging system", SPIE, vol. 3246, 1998, pp. 35-42. cited by applicant . Apple, David J. et al., "Preparation and Study of Human Eyes Obtained Postmortem with the Miyake Posterior Photographic Technique", Ophthalmology, vol. 97, No. 6, 1990, pp. 810-816. cited by applicant . Azzam, Naiel et al., "Long-term lens organ culture system to determine age-related effects of UV irradiation on the eye lens", Experimental Eye Research, 79, 2004, pp. 903-911. cited by applicant . Barak, Adiel et al., "Anterior capsulotomy using the CO.sub.2 laser", SPIE, vol. 3246, 1998, pp. 196-198. cited by applicant . Balaram, Mini et al., Noncontact Specular Microscopy of Human Lens Epithelium, IOVS, vol. 41, No. 2, 2000, pp. 474-481. cited by applicant . Ben-Sira, I. et al., "Clinical method for measurement of light backscattering from the in vivo human lens", Invest. Ophthalmol. Vis. Sci., vol. 19, No. 4 (Reports), 1980, pp. 435-437. cited by applicant . Benjamin, William J., "Borish's Clinical Refraction", W.B. Saunders, publishers, copyright 1998, p. 110. cited by applicant . Bettelheim, Frederick A. et al., "Syneretic Response of Aging Normal Human Lens to Pressure", Investigative Ophthalmology & Visual Science, vol. 44, No. 1, 2003, pp. 258-263. cited by applicant . Bigler, Emmanuel, "Depth of field and Scheimpflug's rule: a "minimalist" geometrical approach", ENSMM, France, 2002, pp. 1-17. cited by applicant . Billie, J. F. et al., "3D Imaging of the Human Eye Using the laser Tomographic Scanner Lts", Institue of Applied Sciences, University of Heidelburg, undated, 2 pgs. cited by applicant . Bito, L.Z. et al., "Age-dependent loss of accommodative amplitude in rhesus monkeys: an animal model for presbyopia", Invest. Ophthalmol. Vis. Sci., vol. 23, No. 1, 1982, pp. 23-31. cited by applicant . Borja, David et al., "Crystalline Lens MTF Measurement During Simulated Accommodation", SPIE, vol. 5688, 2005, pp. 26-32. cited by applicant . Breitling, Detlef et al., "Fundamental aspects in machining of metals with short and ultrashort laser pulses", SPIE, vol. 5339, pp. 1-15. cited by applicant . Burd, H.J. et al., "Can reliable values of Young's modulus be deduced from Fisher's (1971) spinning lens measurements?", Vision Research, 2005, pp. 1-15. cited by applicant . Burd, H.J. et al., "Numerical modeling of the accommodating lens", Vision Research, vol. 42, 2002, pp. 2235-2251. cited by applicant . Carey, James et al., "Propagation and Characterization of Ultrashort Laser Pulses", Spectroscopy of Systems with Spatially Confined Structures, Ed. Rino Di Bartolo, Kluwer Academic Press, Netherlands, 2003, pp. 1-30. cited by applicant . Chen, Wei-Li et al., Ultrasound Biomicroscopic Findings in Rabbit Eyes Undergoing Scleral Suction during Lamellar Refractive Surgery, IOVS, vol. 43, No. 12, 2002, pp. 3665-3672. cited by applicant . Claflin, E. S. et al., "Configuring an electrostatic membrane mirror by least-squares fitting with analytically derived influence functions", J. Opt. Soc. Am. A., vol. 3, No. 11, 1986, pp. 1833-1839. cited by applicant . Coleman, D. Jackson et al., "Presbyopia, Accommodation, and the Mature Catenary", Ophthalmology, vol. 108, No. 9, 2001, pp. 1544-1551. cited by applicant . Crawford, Kathryn S. et al., "The Role of the Iris in Accommodation of Rhesus Monkeys", Investigative Ophthalmology & Visual Science, vol. 31, No. 10, 1990, pp. 2185-2190. cited by applicant . Croft, Mary Ann et al., Accommodative Ciliary Body and Lens Function in Rhesus Monkeys, I: Normal Lens, Zonule and Ciliary Process Configuration in the Iridectomized Eye, IOVS, vol. 47, No. 3, 2006, pp. 1076-1086. cited by applicant . Croft, Mary Ann et al., "Accommodation and Presbyopia", Int Ophthalmol Clin, vol. 41, pp. 33-46. cited by applicant . Croft, Mary Ann et al., "The Zonula, Lens, and Circumlental Space in the Normal Iridectomized Rhesus Monkey Eye", IOVS, vol. 47, No. 3, 2006, pp. 1087-1095. cited by applicant . Croft, Mary Ann et al., "Accommodation and Presbyopia: The Ciliary Neuromuscular View", Opthalmol Clin N Am, vol. 19, 2006, pp. 13-24, ophthalmology.theclinics.com. cited by applicant . Czygan, G. et al., "Mechanical testing of isolated senile human eye lens nuclei", Med. Eng. Phys., vol. 18, No. 5, 1996, pp. 345-349. cited by applicant . Datta, Debajyoti, "Tissue Surgery and Subcellular Photodisruption with Femtosecond Laser Pulses", Thesis for Dept. of Physics, Harvard University, 2002, pp. 1-74. cited by applicant . Dausinger, Friedrich et al., "Micro-machining with ultrashort laser pulses: From basic understanding to technical applications", SPIE, No. 5147, 2002, pp. 1-10. cited by applicant . Dholakia, Sheena A. et al., "Prospective evaluation of phacoemulsification in adults younger than 50 years", J Cataract Refract Surg, vol. 31, 2005, pp. 1327-1333. cited by applicant . Douven, Lucen F.A. et al., "Characterisation of Mechanical Behaviour of Human Skin In Vivo", SPIE, vol. 3914, 2000, pp. 618-629. cited by applicant . Ehrmann, Klaus et al., "Evaluation of porcine crystalline lenses in comparison with molded polymer gel lenses with an improved ex vivo accommodation simulator", SPIE, vol. 5688, 2005, pp. 240-251. cited by applicant . Ehrmann, Klaus et al., "Ex Vivo Accommodation Simulator II--Concept and Preliminary Results", SPIE, vol. 5314, 2004, pp. 48-58. cited by applicant . El-Osta, Austen A.R. et al., "In vitro model for the study of human posterior capsule opacification", J Cataract Refract Surg, vol. 29, 2003, pp. 1593-1600. cited by applicant . Erpelding, Todd N. et al., "Bubble-Based Acoustic Radiation Force for Monitoring Intraocular Lens Elasticity", IEEE Ultrasonics Symposium, 2004, pp. 732-735. cited by applicant . Findl, Oliver et al., "Laserinterferometric Assessment of Pilocarpine-Induced Movement of an Accommodating Intraocular Lens--A Randomized Trial", Ophthalmology, vol. 111, No. 8, 2004, pp. 1515-1521. cited by applicant . Fisher, R.F. et al., "Changes in lens fibres after damage to the lens capsule", Lens Clinic, St. May's Hospital, London, undated, 4 pgs. cited by applicant . Fisher, R.F., "The Elastic Constants of the Human Lens", J. Physiol., vol. 212, 1970, pp. 147-171. cited by applicant . Fisher, R.F., "Presbyopia and the Changes With Age in the Human Crystalline Lens", J. Physiol., vol. 228, 1973, pp. 765-779. cited by applicant . Fisher, R.F., "The Force of Contraction of the Human Ciliary Muscle During Accommodation", J. Physiol., vol. 270, 1977, pp. 51-74. cited by applicant . Foster, C. Stephen et al., "Smolin and Thoft's the Cornea: Scientific Foundations and Clinical Practice", The New England Journal of Medicine, 353:23, 2005, 2 pgs. cited by applicant . Fujimoto, James et al., "Biomedical Optics", Photonics West, SPIE, vol. 5686, 2005, pp. 23-70. cited by applicant . Gayen, Tapan K. et al., "Near-infrared laser welding of aortic and skin tissues and microscopic investigation of welding efficacy", SPIE, vol. 4949, 2003, pp. 182-185. cited by applicant . Gershenzon, A. et al., "Clinical and Epidemiology--New software for lens retro-illumination digital image analysis", Australian and New Zealand Journal of Ophthalmology, 1999, vol. 27, pp. 170-172. cited by applicant . Glasser, Adrian et al., "Accommodative Changes in Lens Diameter in Rhesus Monkeys", IOVS, vol. 47, No. 1, 2006, pp. 278-286. cited by applicant . Glasser, Adrian et al., "On modeling the causes of presbyopia", Vision Research, 2001, vol. 41, pp. 3083-3087. cited by applicant . Glasser, Adrian et al., "Presbyopia and the Optical Changes in the Human Crystalline Lens with Age", Vision Res., 1998, vol. 38, No. 2, pp. 209-229. cited by applicant . Glasser, Adrian et al., "Ultrasound Biomicroscopy of the Aging Rhesus Monkey Ciliary Region", Optometry and Vision Science, 2001, vol. 78, No. 6, pp. 417-424. cited by applicant . Grace, Jeffery M. et al., "Repetitively Pulsed Ruby Lasers as Light Sources for High-Speed Photography", Optical Engineering, vol. 37, No. 8, 1998, pp. 1-26. cited by applicant . Gwon, Arlene et al., "Focal laser photophacoablation of normal and cataractous lenses in rabbits: Preliminary report", J Cataract Refract Surg, vol. 21, 1995, pp. 282-286. cited by applicant . Hamaoui, Marie et al., "Ex-vivo testing of crystalline lens substitutes: a pilot study", SPIE, vol. 3908, 2000, pp. 123-130. cited by applicant . Hammer, Daniel X. et al., "Dual OCT/SLO Imager with Three-Dimensional Tracker", SPIE, vol. 5688, 2005, pp. 33-44. cited by applicant . Hartwick, Andrew T. E. et al., "Ephitelial activity of hexokinase and glucose-6-phosphate dehydrogenase in cultured bovine lenses recovering from pharmaceutical-induced optical damage", Molecular Vision, vol. 9, 2003, pp. 594-600. cited by applicant . Heisterkamp, Alexander et al., "Nonlinear effects inside corneal tissue after fs-photodisruption", SPIE, vol. 4433, 2001, pp. 55-60. cited by applicant . Heisterkamp, Alexander et al., "Pulse energy dependence of subcellular dissection by femtosecond laser pulses", Optics Express, vol. 13, No. 10, 2005, pp. 3690-3696. cited by applicant . Heys, Karl Robert et al., "Massive increase in the stiffness of the human lens nucleus with age: the basis for presbyopia?", Molecular Vision, vol. 10, 2004, pp. 956-963. cited by applicant . Ho, A. et al., "Feasibility of simultaneous correction of ametropia by varying gel refractive index with phaco-ersatz", SPIE, vol. 4245, 2001, pp. 119-128. cited by applicant . Hoffman, Richard S. et al., "Refractive lens exchange as a refractive surgery modality", Copyright .COPYRGT. Lippincott Williams & Wilkins, pp. 22-28. cited by applicant . Holzer, Mike P. et al., "Corneal flap complications in refractive surgery--Part 1: Development of an experimental animal model", J Cataract Refract Surg, vol. 29, 2003, pp. 795-802. cited by applicant . Holzer, Mike P. et al., "Corneal flap complications in refractive surgery--Part 2: Postoperative treatments of diffuse lamellar keratitis in an experimental animal model", J Cataract Refract Surg, vol. 29, 2003, pp. 803-807. cited by applicant . Huber, G. et al., "Room-temperature 2-pm HO:YAG and 3-pm ER:YAG Lasers", Journal de Physique, undated. 3 pgs. cited by applicant . Hunter, David, "First, Gather the Data", New England Journal of Medicine, 354:4, 2006, pp. 329-331. cited by applicant . Johannesson, Mattias, "Active Range Imaging 2", PhD-Thesis: SIMD architectures for Range and Radar Imaging, Linkoping Studies in Science and Technology, Dissertations No. 399, 2005 pp. 1-34. cited by applicant . Jones, C.E. et al., "Refractive index distribution and optical properties of the isolated human lens measured using magnetic resonance imaging (MRI)", Vision Research, vol. 45, 2005, pp. 2352-2366. cited by applicant . Juhasz, T. et al., "Time-resolved Studies of Plama-Mediated Surface Ablation of Soft Biological Tissue with Near-Infrared Picosecond Laser Pulses", SPIE, vol. 2975, 1997, pp. 271-281. cited by applicant . Kasthurirangan, Sanjeev, "Amplitude dependent accommodative dynamics in humans", Vision Research, vol. 43, 2003, pp. 2945-2956. cited by applicant . Kasthurirangan, Sanjeev, "Influence of Amplitude and Starting Point on Accommodative Dynamics in Humans", IOVS, vol. 46, No. 9, 2005, pp. 3463-3472. cited by applicant . Koretz, Jane F. et al., "Accommodation and Presbyopia in the Human Eye--Changes in the Anterior Segment and Crystalline Lens With Focus", IOVS, vol. 38, No. 3, 1997, pp. 569-578. cited by applicant . Konig, Karsten et al., "Are Femtosecond Lasers Safe for Ophthalmic Applications?", Fraunhofer Institute of Biomedical Technologies, undated, pp. 1-16. cited by applicant . Konig, Karsten et al., "First in vivo animal studies on intraocular nanosurgery and multiphoton tomography with low-energy 80 MHz near infrared femtosecond laser pulses", SPIE, vol. 5314, 2004, pp. 262-269. cited by applicant . Konig, Karsten et al., "Cornea surgery with nanojoule femtosecond laser pulses", SPIE, vol. 5688, 2005, pp. 288-293. cited by applicant . Koopmans, Steven A. et al., "Polymer Refilling of Presbyopic Human Lenses In Vitro Restores the Ability to Undergo Accommodative Changes", IOVS, vol. 44, No. 1, 2003, pp. 250-257. cited by applicant . Koretz, Jane F. et al., "Scheimpflug and high-resolution magnetic resonance imaging of the anterior segment: a comparative study", J. Opt. Soc. am. A, vol. 21, No. 3, 2004, pp. 346-354. cited by applicant . Krag, Susanne, "Biomechanical measurements of the lens capsule", Scandinavian University Theses, 1999. cited by applicant . Krag, Susanne et al., "Mechanical Properties of the Human Posterior Lens Capsule", IOVS, vol. 44, No. 2, 2003, pp. 691-696. cited by applicant . Krauss, Joel et al., "Laser Interactions With the Cornea", Survey of Opthamology A167, vol. 31, No. 1, 1986, pp. 37-53. cited by applicant . Krueger, Ronald R. et al., "Experimental Increase in Accommodative Potential after Neodymium: Yttrium-Aluminum-Garnet Laser Photodisruption of Paired Cadaver Lenses", Ophthalmology, vol. 108, No. 11, 2001, pp. 2122-2129. cited by applicant . Krueger, Ronald R. et al., "First safety study of femtosecond laser photodisruption in animal lenses: Tissue morphology and cataractogenesis", J Cataract Refract Surg, vol. 31, 2005, pp. 2386-2394. cited by applicant . Kurapkien , S. et al., "The relationship of ultrasonic and mechanical properties of human nuclear cataract. A pilot study", Ultragarsas, vol. 54, No. 1, 2005, pp. 1392-2114. cited by applicant . Kuizenga, Dirk J., "FM-Laser Operatiob of the Nd:YAG Laser", IEEE Journal of Quantum Electronics, Bol. 6, No. 11, 1970, pp. 673-677. cited by applicant . Kurtz, Ron et al., "Femtosecond Laser Corneal Refractive Surgery", SPIE, vol. 3591, 1999, pp. 209-219. cited by applicant . Kurtz, Ron et al., "Ophthalmic Applications of Femtosecond Lasers", SPIE, vol. 3616, 1999, pp. 51-65. cited by applicant . Kurtz, Ron M. et al., "Optimal Laser Parameters for Intrastromal Corneal Surgery", SPIE, vol. 3255, 1998, pp. 56-66. cited by applicant . Kuszak, J. R. et al., "A Quantitative Analysis of Sutural Contributions to Variability in Back Vertex Distance and Transmittance in Rabbit Lenses as a Function of Development, Growth, and Age", Optometry and Vision Science, vol. 79, No. 3, 2002, pp. 193-204. cited by applicant . Kuszak, J. R. et al., "Development of lens sutures", Int. J. Dev. Biol., vol. 48, 2004, pp. 889-902. cited by applicant . Kuszak, J. R. et al., "Electron Microscope Observations of the Crystalline Lens", Microcsopy Research and Technique, 1996, vol. 33, pp. 441-479. cited by applicant . Kuszak, J. R. et al., "Fibre cell organization in crystalline lenses", Experimental Eye Research, vol. 78, 2004, pp. 673-687. cited by applicant . Kuszak, J. R. et al., "Quantitative Analysis of Animal Model Lens Anatomy: Accommodative Range is Related to Fiber Structure and Organization", Dept. of Ophthalmology and Pathology, undated, 26 pgs. cited by applicant . Kuszak, J. R. et al., "Suppression of Post-Vitrectomy Lens Changes in the Rabbit by Novel Benzopyranyl Esters and Amides", Exp. Eye Res., vol. 75, 2002, pp. 459-473. cited by applicant . Kuszak, J. R. et al., "The Relationship Between Rabbit Lens Optical Quality and Sutural Anatomy after Vitrectomy", Exp. Eye Res., vol. 71, 2000, pp. 267-281. cited by applicant . Kuszak Jer R. et al., "The Structure of the Vertebrate Lens", Chapter 4, pp. 71-118. cited by applicant . Kuszak, J. R. et al., "The Use of an Ex Vivo Mechanical Stretching Apparatus to Examine Fiber Ultrastructure During Accommodation", Dept. of Ophthalmology, Illinois College of Optometry, undated, 5 pgs. cited by applicant . L'Esperance, Jr. "Opthalmic Lasers Photocoagulation, Photoradiation and Surgery", 2.sup.nd Edition, copyright 1983, The C.V. Mosby Company, pp. 529-538. cited by applicant . Liu, Xinbing et al., "In vivo plasma-mediated ablation as a function of laser pulsewidth", SPIE, vol. 2975, 1997, pp. 282-288. cited by applicant . Loerscher, Hanspeter et al., "Noncontact Trephination of the Cornea Using a Pulsed Hydrogen Floride Laser", American Journal of Ophthalmology, vol. 104, pp. 471-475. cited by applicant . Loesel, Frieder H. et al., "Laser-Induced Optical Breakdown on Hard and Soft Tissues and Its Dependence on the Pulse Duration: Experiment and Model", IEEE Journal of Quantum Electronics, vol. 32, No. 10, 1996, pp. 1717-1722. cited by applicant . Manns, Fabrice et al., "Radius of Curvature and Aspericity of the Anterior and Posterior Surface of Human Cadaver Crystalline Lenses", Science Direct Experimental Eye Research, 78, 2004, pp. 39-51. cited by applicant . Masters, B.R., "Three-dimensional Microscopic Tomographic Imaging of the Cataract in a Human Lens In Vivo", Optics Express 332, vol. 3, No. 9, 1998, pp. 332-338. cited by applicant . Mathias, R.T. et al., "Physiological Properties of the Normal Lens", Physiological Review, vol. 77, No. 1, 1997, pp. 21-50. cited by applicant . Michael, Ralph et al., "Refractive Index of Lens Fiber Membranes in Different Parts of the Crystalline Lens", Proceedings of SPIE, vol. 4611, 2002, pp. 159-164. cited by applicant . Marion, II, John E. et al., "Medical Applications of Ultra-Short Pulse Lasers", SPIE, vol. 3616, 1999, pp. 42-50. cited by applicant . Moffat, B.A. et al., "Age-Related Changes in Refractive Index Distribution and Power of the Human Lens as Measured by Magnetic Resonance Micro-Imaging In Vitro", Vision Research, vol. 42, 2002, pp. 1683-1693. cited by applicant . Myers, Raymond I., "Novel Approaches to Correction of Presbyopia With Laser Modification of the Crystalline Lens", Journal of Refractive Surgery, vol. 14, 1998; pp. 136-139. cited by applicant . Myers, O.D., Raymond I. et al., "Feasibility of Using Lasers to Retard Cataract Development in the Ocular Lens by Restoring Lens Movement"; undated, pp. 1-22. cited by applicant . Neev, Joseph, "Ultrashort Pulse Lasers: A New Tool for Biomedical Applications", SPIE, vol. 3255; pp. 2-7. cited by applicant . Oberheide, Uwe et al., "Therapy Monitoring of Laser Cyclophotocoagulation", Proceedings of SPIE, vol. 4611, 2002, pp. 48-53. cited by applicant . Oriowo, Olanrewaju Matthew, "A Study of Ultraviolet Radiation Effects on Procine Crystalline Lens and Development of a New Assay Methodology for UV Cataractogenesis Investigation", A Thesis Presented to the University of Waterloo, 2000, pp. i-xix and 1-218. cited by applicant . Ostrin, Lisa A. et al., "Effects of Pirenzepine on Pupil Size and Accommodation in Rhesus Monkeys", Investigative Ophthalmology & Visual Science, Oct. 2004, vol. 45, No. 10, pp. 3620-3628. cited by applicant . Ostrin, Lisa A. et al., "The Effects of Phenylephrine on Pupil Diameter and Accommodation in Rhesus Monkeys"; Investigative Ophthalmology & Visual Science, 2004, vol. 45, No. 1, pp. 215-221. cited by applicant . Ostrin, Lisa A, "Comparisons Between Pharmacologically and Edinger-Westphal-Stimulated Accommodation in Rhesus Monkeys", Investigative Ophthalmology & Visual Science, 2005, vol. 46, No. 2, pp. 609-617. cited by applicant . Parel, Jean-Marie et al., "Intraocular Implants for the Surgical Correction of Presbyopia"; In Ophthalmic Technologies X, Proceedings of SPIE, vol. 3908, 2000, pp. 115-122. cited by applicant . Patel, C.K. et al., "The Ageing Lens", Association of Optometrists, City University, London; undated, www.optometry.co.uk; pp. 27-31. cited by applicant . Payne, Peter A. et al., "Ophthalmic Applications of Laser-Generated Ultrasound"; SPIE, vol. 3908, 2000, pp. 13-22. cited by applicant . Peterson, Jennifer A. et al., "Intraocular Pressure Measurement in Cynomolgus Monkeys, Tono-Pen Versus Manometry", Investigative Ophthalmology & Visual Science, 1996, vol. 37, No. 6, pp. 1197-1199. cited by applicant . Qian, Wen et al., "3 Year Simvastatin Treatment and Lens Nuclear Back Scattering"; J Ophthalmol, vol. 84, 2000, pp. 512-516. cited by applicant . Qian, Wen et al., "Universal Opacity Standard for Scheimpflug Photography", Ophthalmic Res, 2000, vol. 32, pp. 292-298. cited by applicant . Ripken, T. et al., "FEM Simulation of the Human Lens Compared to Ex-Vivo Porcine Lens Cutting Pattern: A Possible Treatment of Presbyopia"; undated, 11 pgs. cited by applicant . Ripken, T. et al., "Fs-laser Induced Elasticity Changes to Improve Presbyopic Lens Accommodation", undated, 10 pgs. cited by applicant . Rockwell, B.A. et al., "Safe Use of Ultrashort Lasers"; SPIE, vol. 3616, 1999, pp. 32-39. cited by applicant . Roesner, C.A.D. et al., "Light-Matter Interactions on the FEMTOSECOND Time Scale", Department of Physics and Division of Engineering and Applied Sciences, Harvard University, undated, pp. 1-27. cited by applicant . Rol, Pascal et al., "An Optomechanical Eye Model for Observation of Lens Photoablation"; SPIE, 1997, vol. 2971, pp. 171-174. cited by applicant . Sacks, Zachary S. et al., "Laser Spot Size as a Function of Tissue Depth and Laser Wavelength in Human Sclera", SPIE, 1998, vol. 3255, pp. 67-76. cited by applicant . Scammon, Richard J. et al., "Simulations of Shock Waves and Cavitation Bubbles Produced in Water by Picosecond and Nanosecond Laser Pulses", SPIE, 1998, vol. 3254, pp. 264-275. cited by applicant . Schachar, Ronald A. MD et al., "Mechanism of Human Accommodation as Analyzed by Nonlinear Finite Element Analysis", Ann Ophthalmol; 2001; vol. 33, No. 2, pp. 103-112. cited by applicant . Schaeffel, Frank, "Kappa and Hirschberg Ratio Measured With an Automated Video Gaze Tracker", Optometry and Vision Science, 2002, vol. 79, No. 5, pp. 329-334. cited by applicant . Schaffer, Chris B. et al., "Morphology of Femtosecond Laser-Induced Structural Changes in Bulk Transparent Materials", Applied Physics Letters, vol. 84, No. 9, 2004, pp. 1441-1443. cited by applicant . Schaffer, Chris B. et al., "Dynamics of Femtosecond Laser-Induced Breakdown in Water From Femtoseconds to Microseconds", Optics Express, 2002, vol. 10, No. 3, pp. 196-203. cited by applicant . Shen, Nan; "Photodisruption in Biological Tissues Using Femtosecond Laser Pulses", A Thesis Presented to the Department of Physics, Harvard University, 2003, pp. 1-125. cited by applicant . Shen, Nan, et al., "Ablation of Cytoskeletal Filaments and Mitochondria in Live Cells Using a Femtosecond Laser Nanoscissor", MCB, 2005, vol. 2, No. 1, pp. 17-25. cited by applicant . Shen, Nan, et al., "Photodisruption in Biological Tissues and Single Cells Using Femtosecond Laser Pulses", undated, 2 pgs. cited by applicant . Shen, Nan, et al., "Surface and Bulk Photodisruption in Turbid Tissue Using Femtosecond Laser Pulses", Department of Physics and Division of Engineering and Applied Sciences, Harvard University, undated, pp. 1-24. cited by applicant . Sher, Neal A., MD, "Hyperopic Refractive Surgery", Current Opinion in Ophthalmology, 2001, vol. 12, pp. 304-308. cited by applicant . Sivak, Jacob G., "Through the Lens Clearly: Phylogeny and Development, The Proctor Lecture", Opthalmology & Visual Science, 2004, vol. 45, No. 3, pp. 740-747. cited by applicant . Slingsby, Christine, "Lens Crystallin Crystal Structures", undated article. 3 pgs. cited by applicant . Soderberg, Per G., et al., "Angular Dependence of the Intensity of Back Scattered Light From Human Lenses With Nuclear Cataract, Implications for Measurement", SPIE, 2000, vol. 3908, pp. 34-37. cited by applicant . Soderberg, Per G., et al., "External Standard for Measurements with the Scheimpflug Slitlamp Microscope", SPIE, 1997, vol. 2971, pp. 8-13. cited by applicant . Solomon, Ira Seth, M.D., "Aqueous Humor Dynamics", undated, 17 pgs. cited by applicant . Srinivasan R. et al., "Excimer Laser Surgery of the Cornea", American Journal of Ophthalmology, vol. 96, 1993, pp. 710-715. cited by applicant . Stitzel, Joel D., et al., "A Nonlinear Finite Element Model of the Eye With Experimental Validation for the Prediction of Globe Rupture", Stapp Car Crash Journal, 2002, vol. 45, 24 pgs. cited by applicant . Stitzel, Joel D., et al., "Blunt Trauma of the Aging Eye", Arch Ophthalmol, 2005, vol. 123, pp. 789-794. cited by applicant . Strauss, Moshe, et al., "Two-Dimensional Rayleigh Model of Vapor Bubble Evolution", SPIE, 1999, vol. 3601, pp. 212-224. cited by applicant . Strenk, Susan A., et al, "Age-Related Changes in Human Ciliary Muscle and Lens: A Magnetic Resonance Imaging Study", Investigative Ophthalmology & Visual Science, 1999, vol. 40, No. 6, pp. 1162-1169. cited by applicant . Strenk, Susan A., et al, "The Mechanism of Presbyopia", Progress in Retinal and Eye Research, 2004 vol. 11, pp. 1-15. cited by applicant . Strenk, Susan A. et al., "Magnetic Resonance Imaging Study of the Effects of Age and Accommodation on the Human Lens Cross-Sectional Area", IOVS, 2004, Vo. 45, No. 2, pp. 539-545. cited by applicant . Sweeney, Matthew H.J., et al., "Movement of Cysteine in Intact Monkey Lenses: The Major Site of Entry is the Germinative Region", Experimental Eye Research, 2003, vol. 77. pp. 245-251. cited by applicant . Taboada, J. et al., "Response of the Corneal Epithelium to KrF Excimer Laser Pulses", Health Physics, vol. 30, 1981, pp. 677-683. cited by applicant . Tahi, Hassan, et al., "Restoring Accommodation: Surgical Technique and Preliminary Evaluation in Rabbits", SPIE, 1999, vol. 3591, pp. 267-269. cited by applicant . Tang, Daxin; "Influence of Age, Diabetes, and Cataract on Calcium, Lipid-Calcium, and Protein-Calcium Relationships in Human Lenses", Investigative Ophthalmology & Visual Science, 2003, vol. 44, No. 5, pp. 2059-2066. cited by applicant . Tsai, Philbert S., "All-Optical, In-Situ Histology of Neuronal Tissue with Femtosecond Laser Pulses", Imaging in Neuroscience and Development, CSHL Press, undated, 12 pgs. cited by applicant . Vilupuru, Abhiram S., "Spatially Variant Changes in Lens Power During Ocular Accommodation in a Rhesus Monkey Eye", Journal of Vision, 2004, vol. 4, pp. 299-309. cited by applicant . Vilupuru, Abhiram S., "Optical and Biometric Relationships of the Isolated Pig Crystalline Lens", Ophthal. Physiol. Opt., 2001, vol. 21, No. 4, pp. 296-311. cited by applicant . Vogel, Alfred, et al., "Interaction of Laser-Produced Cavitation Bubbles With an Elastic Tissue Model", SPIE, 2001, vol. 4257, pp. 167-177. cited by applicant . Vogel, Alfred, et al., "Numerical Simulation of Optical Breakdown for Cellular Surgery at Nanosecond to Femtosecond Time Scales", SPIE, 2001, vol. 4433, pp. 70-80. cited by applicant . Vogel, Alfred, et al., "Laser-Induced Breakdown in the Eye at Pulse Durations From 80 ns to 100 fs", SPIE, 1998, vol. 3255, pp. 34-49. cited by applicant . Vogel, Alfred, et al; "Kinetics of Phase Transitions in Pulsed IR Laser Ablation of Biological Tissues", SPIE, 2003, vol. 4961, pp. 66-74. cited by applicant . Werner, Liliana, MD, et al., "Capsular Bag Opacification After Experimental Implantation of a New Accommodating Intraocular Lens in Rabbit Eyes", J Cataract Refract Surg, 2004, vol. 30, pp. 1114-1123. cited by applicant . Werner, Liliana, MD. et al., "Posterior Capsule Opacification in Rabbit Eyes Implanted With 1-Piece and 3-Piece Hydrophobic Acrylic Intraocular Lenses", J Cataract Refract Surg, 2005, vol. 31, pp. 805-811. cited by applicant . Ziebarth, Noel, et al; "Non-contact Optical Measurement of Lens Capsule Thickness During Simulated Accommodation", SPIE, 2005, vol. 5688. pp. 19-25. cited by applicant . Faraggi, E. et al., "Stress confinement, shock wave formation and laser induced damage", Conference 5695: Optical Interactions with Tissue and Cells XVI, Photonics West, undated, 1 pg. cited by applicant . Fisher, R F, "The ciliary body in accommodation", Trans Ophthalmol Soc. UK, 1989, 105 (Pt2):208-19,1 pg. cited by applicant . Fisher, RF. "The mechanics of accommodation in relation to presbyopia", Eye, 1988, 2 (Pt6):646-9, 1 pg. cited by applicant . Garner, LF et al., "Changes in equivalent and gradient refractive index of the crystalline lens with accommodation", Optom Vis. Sci., 1997, 74(2):114-9,1 pg. cited by applicant . Garner LF et al., "Changes in ocular dimensions and refraction with accommodation", Ophthalmic Physiol. Opt., 1997, 17(1):12-7, 1 pg. cited by applicant . Helsterkamp, A. et al., "Nanosurgery in live cells using ultrashort laser pulses", Conference 5695: Optical Interactions with Tissue and Cells XVI, Photonics West, undated, 1 pg. cited by applicant . Kuszak, J.R., "Progressively More Complex Star Sutures Formed oin Primate Lenses During Periods of Development, Growth and Aging Are Related to Accommodation", Abstracts Online, obtained from the Internet on Apr. 19, 2006 at: http://www.abstractsonline.com/viewer/viewAbstractPrintFriendly.- asp?CKey={C8FDF5D . . . Apr. 19, 2006, I page. cited by applicant . McBrien NA et al., "Experimental myopia in a diurnal mammal (Sciurus carolinensis) with no accommodative ability", J Physiol., 1993, 469:421-41, 1 pg. cited by applicant . McCourt ME et al., "Refractive state, depth of focus and accommodation of the eye of the California ground squirrel (Spermophilus beecheyi)", Vision Res., 1984, 24(10):1261-6, 1 pg. cited by applicant . Prokofeva GL et al., Effects of low-intensity infrared laser irradiation on the eye an experimental study, Vestn Oftalmol., 1996, 112(1):31-32. 1 pg. cited by applicant . Rafferty, NS et al., "Comparative study of actin filament patterns in lens epithelial cells, Are these determined by the mechanisms of lens accommodation?", Curr Eye Res., 1989, 8(6):569-79, 1 pg. cited by applicant . Van Alphen GW et al., "Elasticity of tissues involved in accommodation", Vision Res., 1991, 31(7-8):1417-38, 1 pg. cited by applicant . Wang, B. et al., "In-vivo animal studies on intraocular nanosurgery with low-energy 80 MHZ near infrared femtosecond laser pulses", Conference 5695: Optical Interactions with Tissue and Cells XVI, Photonics West, undated, 1 pg. cited by applicant . Kuszak et al., "Light, scanning and electron micrographs have lead to the following interpretations of secondary fiber formation", 2004, 16 pgs. cited by applicant . Lubatschowski, H. et al., "Treatment of Presbyopia by Cutting the Cystaline Lens: A Comparison of FEM Simulation and Ex vivo Studies", Lazer Zentrum Hannover e. V. cited by applicant . "Principles of Ultrafast Laser Surgery Femtosecond Laser-Tissue Interaction", copyright .COPYRGT. Center for Ultrafast Optical Sciences, Un of Michigan, undated, 3 pgs. cited by applicant . "Presbyopia--preconditions", Laser Zentrum Hannover e . . . , undated, 11 pgs. cited by applicant . Interalase brochure: The Essential Component of Better Vision. cited by applicant . Gattass, Rafael et al., "Femtosecond laser micromaching Applications in Technology and Biology", Photonics West conference Jan. 2005, 78 pgs. cited by applicant . Mazur, Eric, "An Introduction to Femtosecond Laser Science", Photonics West conference Jan. 2005, 291 pgs. cited by applicant . Nebel, Achim et al., "Fast Micromachining using Picosecond Lasers", Photonics West conference Jan. 2005, 37 pgs. cited by applicant . Hermans E. et al., "Estimating the External Force Acting on the Human Eye Lens During Accommodation Using Finite Elements Modeling", presentation on Accommodation & Presbyopia, May 2005, 1 pg. cited by applicant . Shen, J. et al. "Measurement of the Lens Capsule Contraction Force in the Radial Direction", presentation on Accommodation & Presbyopia, May 2005, 1 pg. cited by applicant . Avro, "Statement for the Use of Animals in Ophthalmic and Visual Research", The Association for Research in Vision and Ophthalmology, copyright .COPYRGT. 2002, obtained from the Internet on Jan. 15, 2005 at: http://www.avro.org/AboutAvro/animalst.asp, 3 pgs. cited by applicant . OSN SuperSite, "Increase in leans stiffness with age may cause presbyopia, study suggests", 2005, 1 pg. cited by applicant . Figure 4.2--Optical constants for a "standard eye", undated, 1 pg. cited by applicant . Picture of an eye obtained from the Internet on Mar. 28, 2005 at: http://www.opt.uh.edu/research/aglasser/aao/gonioani.gif, 1 pg. cited by applicant . Pictures of eyes, 5 pgs. cited by applicant . Loesel paper graphs, 2 pgs. cited by applicant . CD-ROM containing seven videos relating to eyes: 1. AG.MOV 2. Glasser.WMV 3. Kuszak & Zoltoski movie1.mov 4. Kuszak & Zoltoski movie2.mov 5. Kuszak & Zoltoski movie3.mov 6. VidepClip1.mov 7. VideoClip2.mov. cited by applicant . Breitenfeld, R., et al., Finite Element Method-Simulation of the Human Lens during Accomodation, Proc. SPIE Therapuetic Laser Applications and Laser-Tissue Interactions II, vol. 5863, (2005) 9 pgs. cited by applicant . Ripken, T., et al., First in-vivo studies of presbyopia treatment with ultrashort laser pulses, Proc. SPIE 5142, 137, (2003) 9 pgs. cited by applicant . Ripken, T., et al., Investigations for the correction of presbyopia by fs-laser induced cuts, Proc. SPIE 5314, 27, (2004) 9 pgs. cited by applicant . Gills, James P., "Treating astigmatism at the time of cataract surgery", Current Opinion in Ophthalmology, 2002, vol. 13, p. 2-6. cited by applicant . Nichamin, Louis D., "Treating astigmatism at the time of cataract surgery", Current Opinion in Ophthalmology, 2003, vol. 14, p. 35-38. cited by applicant . Chinese Office Action for related application No. CN 200780009762.6, dated Mar. 2, 2011, 10 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2011/023159, dated Mar. 16, 2011, 6 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2011/023117, dated Mar. 25, 2011, 10 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2011/22859, dated Apr. 4, 2011, 7 pgs. cited by applicant . Vogel, Alfred et al., "Intraocular Photodisruption With Picosecond and Nanosecond laser Pulses: Tissue Effects in Cornea, Lens and Retina", Investigative Ophthalmology & Visual Science, Jun. 1994, No. 7, vol. 35, pp. 3032-3044. cited by applicant . Krueger et al., "Experimental Increase in Accommadative Potential After Neodymium:Yttrium-Aluminum-Garnet Laser Photodisruption of Paired Cadaver Lenses", Ophthalmology, vol. 108, No. 11, Nov. 2001, pp. 2122-2129. cited by applicant . Vogel, Alfred et al., "Intraocular Photodisruption With Picosecond and Nanosecond Laser Pulses: Tissue Effects in Cornea, Lens and Retina", Investigative Ophthalmology & Visual Science, Jun. 1994, vol. 35, No. 7, pp. 3032-3044. cited by applicant . Chinese Office Action for related application No. CN 200780009762.6, dated Sep. 9, 2010, 9 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2010/041324, dated Sep. 23, 2010, 11 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2010/041286, dated Sep. 14, 2010, 8 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2010/042582, dated Sep. 20, 2010, 10 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2010/043255, dated Sep. 16, 2010, 10 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2010/043117, dated Sep. 10, 2010, 14 pgs. cited by applicant . Author unknown, "Statement of the Use of Animals in Opthalmic and Visual Research", The Association for Research in Vision and Opthalmology, Obtained from the Internet at: http''//www.avro.org/aboutavro as of Nov. 18, 2010, 3 pgs. cited by applicant . Brian, G. et al., "Cataract Blindness--Challenges for the 21.sup.st Century", Bulletin of the World Health Origination, vol. 79, No. 3, 2001, pp. 249-256. cited by applicant . Eisner, Georg, "Eye Surgery--An Introduction to operative technique", Springer-Verlag, Berlin, 1980, pp. 14-19. cited by applicant . Garner, LF et al., "Changes in Equivalent and Gradient Refractive Index of the Crystalline Lens with Accommodation", Optom, Vis. Sci., vol. 72, No. 2, Feb. 1997, pp. 114-119. cited by applicant . Garner, LF et al., "Changes in Ocular Dimensions and Refraction with Accommodation", Ophthal. Physiol. Opt., vol. 17, No. 1, 1997, pp. 12-17. cited by applicant . Glasser, A. et al., "Biometric, optical and physical changes in the isolated human crystalline end with age in relation to presbyopia", Vision Research, vol. 39, 1999, pp. 1991-2015. cited by applicant . Glasser, A. et al., "On the potential causes of presbyopia", Vision Research, vol. 39, 1999, pp. 1267-1272. cited by applicant . Hanson SSRA et al., "The major in vivo modifications of the human water insoluble lens crystalline are disulfide bonds, desmidation, methoinine oxidation and backbone cleavage", Exp. Eye Res., vol. 71, 2000, pp. 195-207. cited by applicant . Juhasz, T. et al. "Time resolved observations of shock waves and cavitatin bubbles generated by femtosecond laser pulses in corneal tissue and water", Lasers in Surgery and Med, vol. 19, 1996, pp. 23-31. cited by applicant . Krueger, R.R., "Surf's Up--Catch a wave with a waterjet",Jrn. Ref. Surg., vol. 14, No. 6, May/Jun. 1998, pp. 280-281. cited by applicant . Kuszak, Jr et al., "The interrelationship of lens anatomy and optical quality II Primate Lenses", Exp. Eye Res., vol. 59, 1994, pp. 521-535. cited by applicant . Lubatschowski, Holger, "Surgical Laser System for the Treatment of Presbyopia", 7.sup.th Biotech in Europe Investor Forum, Switzerland, Oct. 2-3, 2007, 9 pgs. cited by applicant . McBrien, N. A et al., "Experimental Myopia in a Diumal Mammal (Sciurus carolinesis) with No Accommodative Ability", J. Physiol., vol. 469, 1993, pp. 427-441. cited by applicant . McCourt, M. E et al., Refractive State, Depth of Focus, and Accommodation of the Eye of the California ground squirrel (Spermophiliu beecheyi), Vision Res, vol. 24, No. 10, 1984, pp. 1261-1266. cited by applicant . Prokofeva, G. I et al., "Effects of Low-Intensity Infrared Laser Irradiation on the Eye, (An Experimental Study)", Vestn. Oftalmol., vol. 112, No. 1, 1996, pp. 31-32, with English Abstract, 5 pgs. cited by applicant . Sliney, D. H et al., "Medical Lasers and Their Safe Use", Springer Verlag, New York, 1993, pp. 42-50. cited by applicant . International Search Report for related application No. PCT/US2011/56279,dated Feb. 1, 2012, 9 pgs. cited by applicant . Unpublished U.S. Appl. No. 13/273,653, filed Oct. 14, 2011 (31 pgs). cited by applicant . Unpublished U.S. Appl. No. 13/427,130, filed Mar. 22, 2012 (34 pgs). cited by applicant . Unpublished U.S. Appl. No. 13/427,149, filed Mar. 22, 2012 (29 pgs). cited by applicant . Unpublished U.S. Appl. No. 13/427,319, filed Mar. 22, 2012 (32 pgs). cited by applicant . Unpublished U.S. Appl. No. 13/435,103, filed Mar. 30, 2012 (72 pgs). cited by applicant . Hammer, Daniel et al., "Shielding Properties of Laser-Induced Breakdown in Water for Pulse Durations From 5 ns to 125 fs", Applied Optics, 1997, vol. 36, No. 22, pp. 5630-5640. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2012/030247,dated Jul. 9, 2012, 6 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2012/030059,dated Jul. 13, 2012, 12 pgs. cited by applicant . International Search Report and Written Opinion for related application No. PCT/US2012/030259,dated Jul. 13, 2012, 11 pgs. cited by applicant . European Search Report, Application No. 07718200, dated Mar. 4, 2015. cited by applicant . Sep. 25, 2017, PCT, WO2007_7084579 Seach Report and Opinion. cited by applicant . Feb. 19, 2018, EPO, EP 07 718 200.4 Search and Exam Report. cited by applicant . Jan. 2, 2008, PCT, PCT/US2007/001353 Search Report and Opinion. cited by applicant . Oct. 23, 2007, PCT, PCT/US2007/001312 Search Report and Opinion. cited by applicant . Sep. 25, 2007, PCT, PCT/US2007/001262 Search Report and Opinion. cited by applicant . Oct. 4, 2007, PCT, PCT/US2007/001486 Search Report and Opinion. cited by applicant . Sep. 10, 2010, PCT, PCT/US2010/043117 Search Report and Opnion. cited by applicant . Feb. 6, 2018, EPO, EP 07 718 259.0 Search and Exam Report. cited by applicant. |
Primary Examiner: Eiseman; Lynsey C
Attorney, Agent or Firm: Belvis; Glen P. Belvis Law, LLC.
Claims
What is claimed:
1. A method for delivering a laser beam to a lens of an eye comprising: a. providing a laser beam from a laser in a laser delivery system; b. the laser delivery system defining an optical path, whereby the laser delivery system directs the laser beam along the optical path from the laser to the lens of the eye; wherein components are located in the optical path, the components comprising: an x y scanner; a z focus mechanism; and, a reference; wherein the reference is configured for use in making a laser lens positional determination; c. the laser delivery system determining the shape and position of the lens with respect to the laser: (i) based upon the reference and (ii) based upon mathematical modeling and observation data; and, d. the laser delivery system automatically focusing the laser beam to a location in the lens of the eye; wherein the location is selected based upon the determinations of step c.
2. The method of claim 1, wherein the reference is a reference mark and is located on a patient interface device.
3. The method of claim 1, comprising directing the laser beam in the lens of the eye in a predetermined shot pattern; the lens defining a shape; the shot pattern comprising a series of shots that form a volumetric shaped removal, the volumetric shaped removal being positioned entirely within the lens and essentially following the shape of the lens.
4. The method of claim 1, comprising the step of directing the laser beam in a shot pattern to from an annular ring shaped capsulorhexis.
5. The method of claim 4, comprising: directing the laser beam in the lens of the eye in a predetermined shot pattern, the shot pattern comprising a series of shots that form a grid cut pattern: removing the lens material; and, replacing the lens material.
6. A method for delivering a laser beam to a lens of an eye comprising: a. providing a laser beam from a laser in a laser delivery system; the laser delivery system further comprising a lens model and a control system; b. providing to the laser delivery system observation data of a position of the lens with respect to the laser system; the laser delivery system determining the position and shape of a structure of the lens based on the lens model and the observed data; c. the laser delivery system automatically directing the laser beam in the lens of the eye in a pattern of shots; d. wherein the pattern of shots is based upon the determined position and shape of the structure of the lens; e. the laser delivery system automatically focusing a shot of the shot pattern in the lens of the eye based upon the determination of step b.
7. The method of claim 6, comprising directing the laser beam in the lens of the eye in a predetermined shot pattern, the shot pattern comprising as series of shots that form a volumetric shaped removal, the volumetric shaped removal being positioned entirely within the lens and essentially following a shape of the lens.
8. The method of claim 6, comprising directing the laser beam in a shot pattern to form an annular ring shaped capsulorhexis.
9. A method for delivering a laser beam to a lens of an eye comprising: a. determining a position of the lens of the eye with respect to a fixed reference in a laser beam delivery system; and determining a shape and the position of an outer surface of the lens of the eye based upon modeling data and observation data, wherein the laser beam delivery system is configured to deliver a laser beam along an optical path from a laser to the lens of the eye; wherein components are located along the optical path, the components comprising: an x y scanner; a z focus mechanism; and the fixed reference; b. the laser beam delivery system directing the laser beam to the lens of the eye along the optical path; c. the laser beam delivery system automatically directing the laser beam in the lens of the eye in a predetermined shot pattern, the shot pattern comprising as series of shots that form a volumetric shape; and, d. the volumetric shape being positioned at a location entirely within the lens of the eye; wherein the location within the lens of the eye is based upon the determined position and shape of the outer surface of the lens of the eye.
10. A method of directing a laser beam to the lens of the eye comprising: a. providing observed lens data to a laser beam delivery system; the laser beam delivery system comprising: (i) optical path components defining an optical path; (ii) wherein the optical path components comprise an x y scanner, a z focus, and a fixed reference; and, (iii) modeled lens data; b. based upon the modeled lens data, the fixed reference, and the observed lens data the laser beam delivery system determining a shape and a position of the lens, wherein the observed data is obtained from a light source; and, c. the laser beam delivery system directing a laser beam to the lens of the eye in a laser beam pattern, based upon the determined shape and the determined position of the lens, wherein the laser beam is directed along the optical path.
Description
BACKGROUND OF THE INVENTION
The present invention relates to systems and methods for treating the structure of the natural human crystalline lens with a laser to address a variety of medical conditions such as presbyopia, refractive error and cataracts and combinations of these.
The anatomical structures of the eye are shown in general in FIG. 1, which is a cross sectional view of the eye. The sclera 131 is the white tissue that surrounds the lens 103 except at the cornea 101. The cornea 101 is the transparent tissue that comprises the exterior surface of the eye through which light first enters the eye. The iris 102 is a colored, contractible membrane that controls the amount of light entering the eye by changing the size of the circular aperture at its center (the pupil). The ocular or natural crystalline lens 103, a more detailed picture of which is shown in FIGS. 1A-F, (utilizing similar reference numbers for similar structures) is located just posterior to the iris 102. The terms ocular lens, natural crystalline lens, natural lens, natural human crystalline lens, and lens (when referring to the prior terms) are used interchangeably herein and refer to the same anatomical structure of the human eye.
Generally, the ocular lens changes shape through the action of the ciliary muscle 108 to allow for focusing of a visual image. A neural feedback mechanism from the brain allows the ciliary muscle 108, acting through the attachment of the zonules 111, to change the shape of the ocular lens. Generally, sight occurs when light enters the eye through the cornea 101 and pupil, then proceeds through the ocular lens 103 through the vitreous 110 along the visual axis 104, strikes the retina 105 at the back of the eye, forming an image at the macula 106 that is transferred by the optic nerve 107 to the brain. The space between the cornea 101 and the retina 105 is filled with a liquid called the aqueous 117 in the anterior chamber 109 and the vitreous 110, a gel-like clear substance, in the chamber posterior to the lens 103.
FIG.1A illustrates, in general, components of and related to the lens 103 for a typical 50-year old individual. The lens 103 is a multi-structural system. The lens 103 structure includes a cortex 113, and a nucleus 129, and a lens capsule 114. The capsule 114 is an outer membrane that region envelopes the other interior structures of the lens. The lens epithelium 123 forms at the lens equatorial 121 generating ribbon-like cells or fibrils that grow anteriorly and posteriorly around the ocular lens. The nucleus 129 is formed from successive additions of the cortex 113 to the nuclear regions. The continuum of layers in the lens, including the nucleus 129, can be characterized into several layers, nuclei or nuclear regions. These layers include an embryonic nucleus 122, a fetal nucleus 130, both of which develop in the womb, an infantile nucleus 124, which develops from birth through four years for an average of about three years, an adolescent nucleus 126, which develops from about four years until puberty which averages about 12 years, and the adult nucleus 128, which develops at about 18 years and beyond.
The embryonic nucleus 122 is about 0.5 mm in equatorial diameter (width) and 0.425 mm in Anterior-Posterior axis 104 (AP axis) diameter (thickness). The fetal nucleus 130 is about 6.0 mm in equatorial diameter and 3.0 mm in AP axis 104 diameter. The infantile nucleus 124 is about 7.2 mm in equatorial diameter and 3.6 mm in AP axis 104 diameter. The adolescent nucleus 126 is about 9.0 mm in equatorial diameter and 4.5 mm in AP axis 104 diameter. The adult nucleus 128 at about age 36 is about 9.6 mm in equatorial diameter and 4.8 mm in AP axis 104 diameter. These are all average values for a typical adult human lens approximately age 50 in the accommodated state, ex vivo. Thus this lens (nucleus and cortex) is about 9.8 mm in equatorial diameter and 4.9 mm in AP axis 104 diameter. Thus, the structure of the lens is layered or nested, with the oldest layers and oldest cells towards the center.
The lens is a biconvex shape as shown in FIGS. 1 and 1A. The anterior and posterior sides of the lens have different curvatures and the cortex and the different nuclei in general follow those curvatures. Thus, the lens can be viewed as essentially a stratified structure that is asymmetrical along the equatorial axis and consisting of long crescent fiber cells arranged end to end to form essentially concentric or nested shells. The ends of these cells align to form suture lines in the central and paracentral areas both anteriorly and posteriorly. The older tissue in both the cortex and nucleus has reduced cellular function, having lost their cell nuclei and other organelles several months after cell formation.
Compaction of the lens occurs with aging. The number of lens fibers that grow each year is relatively constant throughout life. However, the size of the lens does not become as large as expected from new fiber growth. The lens grows from birth through age 3, from 6 mm to 7.2 mm or 20% growth in only 3 years. Then the next approximate decade, growth is from 7.2 mm to 9 mm or 25%; however, this is over a 3 times longer period of 9 years. Over the next approximate 2 decades, from age 12 to age 36 the lens grows from 9 mm to 9.6 mm or 6.7% growth in 24 years, showing a dramatically slowing observed growth rate, while we believe there is a relatively constant rate of fiber growth during this period. Finally, in the last approximately 2 decades described, from age 36 to age 54, the lens grows by a tiny fraction of its youthful growth, from 9.6 to 9.8 mm or 2.1% in 18 years. Although there is a geometry effect of needing more lens fibers to fill larger outer shells, the size of the older lens is considerably smaller than predicted by fiber growth rate models, which consider geometry effects. Fiber compaction including nuclear fiber compaction is thought to explain these observations
In general, presbyopia is the loss of accommodative amplitude. In general refractive error is typically due to variations in the axial length of the eye. Myopia is when the eye is too long resulting in the focus falling in front of the retina. Hyperopia is when the eye is too short resulting in the focus falling behind the retina. In generally, cataracts are areas of opacification of the ocular lens which are sufficient to interfere with vision. Other conditions, for which the present invention is directed, include but are not limited to the opacification of the ocular lens.
Presbyopia most often presents as a near vision deficiency, the inability to read small print, especially in dim lighting after about 40-45 years of age. Presbyopia, or the loss of accommodative amplitude with age, relates to the eyes inability to change the shape of the natural crystalline lens, which allows a person to change focus between far and near, and occurs in essentially 100% of the population. Accommodative amplitude has been shown to decline with age steadily through the fifth decade of life.
Historically, studies have generally attributed loss of accommodation to the hardening of the crystalline lens with age and more specifically, to an increase in the Young's Modulus of Elasticity of the lens material. More recent studies have examined the effect of aging on the relative change in material properties between the nucleus and cortex. These studies have provided varying theories and data with respect to the hardening of the lens. In general, such studies have essentially proposed the theory that the loss of flexibility is the result of an increase in the Young's Modulus of Elasticity of the nucleus and/or cortex material. Such studies have viewed this hardening as the primary factor in the loss of accommodative amplitude with age and hence the cause of presbyopia.
Although the invention is not bound by it, the present specification postulates a different theory of how this loss of lens flexibility occurs to cause presbyopia. In general, it is postulated the structure of the lens rather than the material properties of the lens plays a greater role in loss of flexibility and resultant presbyopia than was previously understood. Thus, contrary to the teachings of the prior studies in this field as set forth above, material elasticity is not the dominate cause of presbyopia. Rather, it is postulated that it is the structure of the lens and changes in that structure with age that is the dominant cause of presbyopia. Thus, without being limited to or bound by this theory, the present invention discloses a variety of methods and systems to provide laser treatments to increase the flexibility of the lens, based at least in part on the structure of the lens and structural changes that occur to the lens with aging. The present invention further discloses providing laser treatments to increase the flexibility of the lens that are based primarily on the structure of the lens and structural changes that occur to the lens with aging.
Accordingly, the postulated theory of this specification can be illustrated for exemplary purposes by looking to and examining a simple hypothetical model. It further being understood this hypothetical model is merely to illustrate the present theory and not to predict how a lens will react to laser pulses, and/or structural changes. To understand how important structure alone can be, consider a very thin plank of wood, say 4 ft by 4 ft square but 0.1 inch thick. This thin plank is not very strong and if held firmly on one end, it does not take much force to bend this thin plank considerably. Now consider five of these same 0.1 inch thickness planks stacked on top of each other, but otherwise not bound or tied together. The strength would increase and for the same force a somewhat smaller deflection will occur. Now, consider taking those same five planks and fastening them together with many screws or by using very strong glue, or by using many C-Clamps to bind them together. The strength of the bound planks is much higher and the deflection seen from the same force would be much smaller.
Without saying this simple model reflects the complex behavior of the lens, we generally hypothesize that when considering a volume of lens material, especially near the poles (AP axis), that is essentially bound by increased friction and compaction due to aging, that separating those bound layers into essentially unbound layers will increase the deflection of those layers for the same applied force and hence increase flexibility of the lens. Applicants, however, do not intend to be bound by the present theory, and it is provided solely to advance the art, and is not intended to and does not restrict or diminish the scope of the invention,
Thus, further using this model for illustration purposes, under the prior theories and treatments for presbyopia, the direction was principally toward the material properties, i.e., Modulus of the material in the stack, rather than on the structure of the stack, i.e., whether the layers were bound together. On the other hand, the presently postulated theory is directed toward structural features and the effects that altering those features have on flexibility.
In general, current presbyopia treatments tend to be directed toward alternatives to increasing the amplitude of accommodation of the natural crystalline lens. These treatments include a new class of artificial accommodative Intraocular Lenses (IOL's), such as the Eyeonics CRYSTALENS, which are designed to change position within the eye; however, they offer only about 1 diopter of objectively measured accommodative amplitude, while many practitioners presently believe 3 or more diopters are required to restore normal visual function for near and far objects. Moreover, researchers are pursuing techniques and materials to refill the lens capsule with synthetic materials. Additionally, present surgical techniques to implant artificial accommodative IOL's are those developed for the more serious condition of cataracts. It is believed that practitioners are reluctant at the present time to replace a patient's clear albeit presbyopic natural crystalline lens, with an accommodative IOL due to the risks of this invasive surgical technique on a patient who may simply wear reading glasses to correct the near vision deficiency. However, developments may offer greater levels of accommodative amplitude in implantable devices and refilling materials. To better utilize such device improvements and to increase the accommodative amplitude of existing implantable devices, improved surgical techniques are provided herein as a part of the present invention.
Refractive error, typically due to the length of the eye being too long (myopia) or to short (hyperopia) is another very common problem effecting about one-half of the population. Laser surgery on the cornea, as proposed by Trokel and L'Esperance and improved by Frey and others, does offer effective treatment of refractive errors but factors such as higher degrees of refractive error, especially in hyperopia, thin corneas or a changing refractive error with time, such as that brought on by presbyopia, limit the clinical use of laser corneal surgery for many.
Cataracts, or the condition when the natural crystalline lens becomes opaque and clouds vision, occurs in millions of people per year and are treated effectively with a surgical techniques such as ultrasonic phacoemulsification pioneered by Kelman 30 years ago. Although the techniques have been refined over the years, safety concerns from ocular trauma, especially to the corneal endothelium from the ultrasonic energy required to break up a hardened cataract is undesirable; especially for those with a compromised corneal endothelium, such as those with Fuchs Dystrophy. Moreover, the use of lasers in the treatment of cataracts has a further issue. Cataracts scatter light, including laser light and thus can prevent a laser treatment beam from having the desired tissue effect. Accordingly, as provided in detail in this specification herein improvements in the delivery of lasers to cataractous tissue are provided.
SUMMARY
Provided herein are embodiments of the present invention. Accordingly, there is provided method and system for delivering a laser beam to a lens of an eye that utilize the steps of providing a laser, an optical path for directing a laser beam from the laser to the lens of the eye, determining the shape and position of the lens with respect to a fixed point, and focusing a laser beam to a location in the lens of the eye, wherein that location was determined based at least in part upon data and/or information from the determining step.
There is further provided a method and system for delivering a laser beam in the lens of the eye in a predetermined shot pattern that utilize as series of shots that form a shell cut, a partial shell cut, a laser suture cut and/or a volumetric shaped removal, which essentially following the shape of a suture layer of the lens, i.e., a layer shape of the lens.
There is further provided a method and system for directing a laser beam in the lens of the eye in a predetermined shot pattern such that a grid cut pattern is formed. The delivery of this grid cut pattern resulting in the formation of cubes, which can then be removed from the lens capsule and a replacement material placed therein.
There is further provided a method and system for delivering a laser beam to a lens of an eye that utilize the steps of providing a laser, determining the shape and position of the lens with respect to a fixed point, directing the laser beam in the lens of the eye in a pattern of shots, which is based in part upon the geometry of a natural human lens and focusing the laser shots in the lens of the eye based in part upon information obtained from the determining step.
There is further provided a system and method for directing a laser beam in a shot pattern to from an annular ring shaped capsulorhexis.
There is further provided a method and system for creating a shell cut, a partial shell cut, a laser suture cut, and/or a volumetric shaped removal within a lens of an eye that utilize the steps of providing a laser, directing the laser beam to the lens of the eye, said lens having an outer surface and said outer surface having a shape, directing the laser beam in the lens of the eye in a predetermined shot pattern, said shot pattern comprising as series of shots that form a shell cut, a partial shell cut, a laser suture cut, and/or a volumetric shaped removal within a lens of an eye and which essentially following the shape of the outer surface of the lens. It is further provided that these shell cuts, partial shell cuts, laser suture cuts, and/or volumetric shaped removals may generally corresponds to a suture layer of the lens selected from the group consisting of suture layers having 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, and fractions between 3 and 15 sutures.
There is further provided a system and method for creating a shell cut and/or partial shell cut within a lens of an eye that utilize the steps of directing a laser beam to the lens of the eye in a predetermined shot pattern that utilize as series of shots that form a shell cut and/or partial shell cut, which has a flower like shape having a contour that generally follows approximately the last 15% of the fiber length from the end of the fiber.
There is further provided a system and method for modifying the gradient index of a lens of an eye that utilize the steps of providing a laser, directing the laser beam to the lens of the eye in a predetermined shot pattern, said shot pattern comprising as series of shots that form at least two shapes of different densities, which shapes are nested within each other, positioned entirely within the lens and follow the outer surface of the lens.
There is further provided a system for treating conditions of the lens comprising a laser, laser focusing optics, a scanner and a control system that has a plurality of means for directing in cooperation with the laser, the scanner and the laser focusing optics, laser shot pattern that provide the ability to performing a lens material extraction, the treatment of presbyopia, and the treatment of refractive error.
There is further provided a system for delivering a laser to an eye and for obtaining stereo images of the eye comprising a laser, focusing optics, a scanner and a camera. Wherein the scanner is optically associated with the laser and the camera so that the scanner has the capability to provide stereo pairs of images of the eye and deliver a laser beam from the laser to the eye.
There is further provided a system for delivering a laser to an eye and for determining the position of the eye comprising a patient support, a laser, optics for delivering a laser beam, a control system for delivering the laser beam to the lens of the eye in a particular pattern, a lens position determination apparatus, and, a laser patient interface.
One of ordinary skill in the art will recognize, based on the teachings set forth in these specifications and drawings, that there are various embodiments and implementations of these teachings to practice the present invention. Accordingly, the embodiments in this summary are not meant to limit these teachings in any way.
BRIEF DESCRIPTION OF THE DRAWINGS
FIGS. 1 and 1A are cross sectional representations of the human eye.
FIG. 2 is a block schematic diagram of a type of system for delivering a laser beam shot pattern to the lens of an eye according to the teachings of the present invention.
FIG. 2A is a block schematic diagram of illustrative components forming a portion of a system for delivering a laser beam shot pattern to the lens of an eye according to the teachings of the present invention.
FIG. 3 is a diagram of the anterior surface of a lens along the AP axis illustrating a laser shot pattern having a flower like shape which has a contour generally following approximately the last 15% of the fiber length from the end of the fiber.
FIGS. 4A, 4B, 4C, 4D and 4E are diagrams representing elevation views of the geometry used for the development of laser shot patterns based upon the structure of the fetal nucleus (three suture branch nucleus) as it is rotated from the posterior view 4A through and to the anterior view 4E.
FIGS. 5A, 5B, and 5C are diagrams representing posterior, side and anterior elevation views, respectively, of the geometry used for the development of laser shot patterns based upon the structure of the infantile nucleus (six suture branch nucleus).
FIGS. 6A, 6B and 6C are diagrams representing posterior, side and anterior elevation views, respectively of the geometry used for the development of laser shot patterns based upon the structure of the adolescent nucleus (nine suture branch nucleus).
FIGS. 7A, 7B and 7C are diagrams representing posterior, side and anterior elevation views, respectively of the geometry used for the development of laser shot patterns based upon the structure of the an adult nucleus (12 suture branch).
FIGS. 8 aid 8A are perspective cutout views of an adult lens representing the placement of essentially concentric shells in accordance with the teachings of the present invention.
FIG. 9 is a cross-section drawing of the lens relating to Burd modeling.
FIG. 10 is a cross-section drawing of a lens based upon Burd modeling.
FIG. 11 is a cross-section drawing of a lens based upon Burd modeling.
FIG. 12 is a cross-section drawing of a lens based upon Burd modeling.
FIG. 13 is a cross-section drawing of a lens showing the placement of a shell laser shot pattern in accordance with the teachings of the present invention.
FIG. 14 is a cross-section drawing of a lens showing the placement of a shell laser shot pattern in accordance with the teachings of the present invention.
FIG. 15 is a cross-section drawing of a lens showing the placement of a partial shell laser shot pattern in accordance with the teachings of the present invention.
FIG. 16 is a cross-section drawing of a lens showing the placement of a partial shell laser shot pattern in accordance with the teachings of the present invention.
FIG. 17 is a cross-section drawing of a lens showing the placement of a shell laser shot pattern in accordance with the teachings of the present invention.
FIGS. 18-24 are cross-section drawings of a lens showing the placement of a volumetric removal laser shot patterns in accordance with the teachings of the present invention.
FIG. 25 is a cross-section drawing of a lens showing the placement of a cube laser shot pattern in accordance with the teachings of the present invention.
FIGS. 26-27 are cross-section drawings of a lens showing the placement of a gradient index modification laser shot patterns in accordance with the teachings of the present invention.
FIGS. 28A, C and E diagrams depicting laser suture cut shot patterns on the anterior portion of a lens of the present invention.
FIGS. 28B, D, and F are diagrams illustrating the placement of the shot patterns of FIGS. 28A, C, and E respectively.
FIG. 29 is a diagram illustrating the relative placement of the shot patterns of FIGS. 28A, C, and E, if performed in the same lens.
FIGS. 30A-D are diagrams of the cross-section of a lens illustrating a capsulorhexis shot pattern of the present invention.
FIGS. 31A to 31D are illustrations of gradient index modifications of the lens in accordance with the present inventions.
DETAILED DESCRIPTION OF THE DRAWINGS AND THE PREFERRED EMBODIMENTS
In general, the present invention provides a system and method for increasing the amplitude of accommodation and/or changing the refractive power and/or enabling the removal of the clear or cataractous lens material of a natural crystalline lens. Thus, as generally shown in FIG. 2 there is provided a system for delivering a laser beam shot pattern to the lens of an eye comprising: a patient support 201; a laser 202; optics for delivering the laser beam 203; a control system for delivering the laser beam to the lens in a particular pattern 204, which control system 204 is associated with and/or interfaces with the other components of the system as represented by lines 205; a means for determining the position of lens with respect to the laser 206, which means 206 receives an image along path 211 of the lens of the eye; and a laser patient interface 207.
The patient support 201 positions the patent's body 208 and head 209 to interface with the optics for delivering the laser beam 203.
In general, the laser 202 should provide a beam 210 that is of a wavelength that transmits through the cornea, aqueous and lens. The beam should be of a short pulse width, together with the energy and beam size, to produce photodisruption. Thus, as used herein, the term laser shot or shot refers to a laser beam pulse delivered to a location that results in photodisruption. As used herein, the term photodisruption essentially refers to the conversion of matter to a gas by the laser. In particular, wavelengths of about 300 nm to 2500 nm may be employed. Pulse widths from about 1 femtosecond to 100 picoseconds may be employed. Energies from about a 1 nanojoule to 1 millijoule may be employed. The pulse rate (also referred to as pulse repetition frequency (PRF) and pulses per second measured in Hertz) may be from about 1 KHz to several GHz. Generally, lower pulse rates correspond to higher pulse energy in commercial laser devices. A wide variety of laser types may be used to cause photodisruption of ocular tissues, dependent upon pulse width and energy density. Thus, examples of such lasers would include: the Delmar Photonics Inc. Trestles-20, which is a Titanium Sapphire (Ti:Sapphire) oscillator having a wavelength range of 780 to 840 nm, less than a 20 femtosecond pulse width, about 100 MHz PRF, with 2.5 nanojoules; the Clark CPA-2161, which is an amplified Ti:Sapphire having a wavelength of 775 nm, less than a 150 femtosecond pulse width, about 3 KHz PRF, with 850 microjoules; the IMRA FCPA (fiber chirped pulse amplification) .mu.jewel D series D-400-HR, which is a Yb:fiber oscillator/amplifier having a wavelength of 1045 nm, less than a 1 picosecond pulse width, about 5 MHz PRF, with 100 nanojoules; the Lumera Staccato, which is a Nd:YVO4 having a wavelength of 1064 nm, about 10 picosecond pulse width, about 100 KHz PRF, with 100 microjoules; and, the IMRA FCPA (fiber chirped pulse amplification) .mu.jewel D series D-400-NC, which is a Yb:fiber oscillator/amplifier having a wavelength of 1045 nm, less than a 100 picosecond pulse width, about 200 KHz PRF, with 4 microjoules.
In general, the optics for delivering the laser beam 203 to the natural lens of the eye should be capable of providing a series of shots to the natural lens in a precise and predetermined pattern in the x, y and z dimension. The optics should also provide a predetermined beam spot size to cause photodisruption with the laser energy reaching the natural lens. Thus, the optics may include, without limitation: an x y scanner; a z focusing device; and, focusing optics. The focusing optics may be conventional focusing optics, and/or flat field optics and/or telecentric optics, each having corresponding computer controlled focusing, such that calibration in x, y, z dimensions is achieved. For example, an x y scanner may be a pair of closed loop galvanometers with position detector feedback. Examples of such x y scanners would be the Cambridge Technology Inc. Model 6450, the SCANLAB hurrySCAN and the AGRES Rhino Scanner. Examples of such z focusing devices would be the Phsyik International Peizo focus unit Model ESee Z focus control and the SCANLAB varrioSCAN.
In general, the control system for delivering the laser beam 204 may be any computer, controller, and/or software hardware combination that is capable of selecting and controlling x y z scanning parameters and laser firing. These components may typically be associated at least in part with circuit boards that interface to the x y scanner, the z focusing device and/or the laser. The control system may also, but does not necessarily, have the further capabilities of controlling the other components of the system as well as maintaining data, obtaining data and performing calculations. Thus, the control system may contain the programs that direct the laser through one or more laser shot patterns.
In general, the means for determining the position of the lens with respect to the laser 206 should be capable of determining the relative distance with respect to the laser and portions of the lens, which distance is maintained constant by the patient interface 207. Thus, this component will provide the ability to determine the position of the lens with respect to the scanning coordinates in all three dimensions. This may be accomplished by several methods and apparatus. For example, x y centration of the lens may i)e accomplished by observing the lens through a coboresighed camera system and display or by using direct view optics and then manually positioning the patients'eye to a known center. The z position may then be determined by a range measurement device utilizing optical triangulation or laser and ccd system, such as the Micro-Epsilon opto NCDT 1401 laser sensor and/or the Aculux Laser Ranger LR2-22. The use of a 3-dimensional viewing and measurement apparatus may also be used to determine the x, y and z positions of the lens. For example, the Hawk 3 axis non-contact measurement system from Vision Engineering could be used to make these determinations. Yet a further example of an apparatus that can be used to determine the position of the lens is a 3-dimension measurement apparatus. This apparatus would comprise a camera, which can view a reference and the natural lens, and would also include a light source to illuminate the natural lens. Such light source could be a structured light source, such as for example a slit illumination designed to generate 3-dimensional information based upon geometry.
A further component of the system is the laser patient interface 207. This interface should provide that the x, y, z position between the natural lens and the laser remains fixed during the procedure, which includes both the measurement steps of determining the x y z position and the delivery step of delivering the laser to the lens in a shot pattern. The interface device may contain an optically transparent applanator. One example of this interface is a suction ring applanator that is fixed against the outer surface of the eye and is then positioned against the laser optical housing, thus fixing the distance between the laser, the eye and the natural lens. The reference marks for the 3-dimensional viewing and measuring apparatus may also be placed on this applanator. A further example of a laser patient interface is a device having a lower ring, which has suction capability for affixing the interface to the eye. The interface further has a flat bottom, which presses against the eye flattening the eye's shape. This flat bottom is constructed of material that transmits the laser beam and also preferably, although not necessarily, transmits optical images of the eye within the visible light spectrum. The upper ring has a structure for engaging with the housing for the laser optics and/or some structure that is of known distance from the laser along the path of the laser beam and fixed with respect to the laser. The flat bottom further has a reference, which consists of three reference marks. Although three marks are provided in this example to make up the reference, the reference may consist of only a single mark or several marks. Further examples of such devices are generally disclosed in US D462442, US D462443, and US D459807S, the disclosures of which are hereby incorporated by reference. As an alternative to an applanator, the interface may be a corneal shaped transparent element whereby the cornea is put into direct contact with the interface or contains an interface fluid between.
An illustrative combination utilizing by way of example specific optics for delivering the laser beam 203 and means for determining the position of the lens 206, is shown in part, in FIG. 2A. FIG. 2A is a more detailed schematic diagram of a configuration of the system of FIG. 2. Thus, the example of FIG. 2A provides a laser 202, laser optics for delivering the laser beam 203, which optics comprise a beam expander telescope 220, a z focus mechanism 221, a beam combiner 222, an x y scanner 223, and focusing optics 224. There is further provided in FIG. 2A relay optics 230, camera optics with zoom and focus 231, and a ccd camera 232, which components form a part of a three-dimensional viewing and measuring apparatus. Moreover, these components 230, 231 and 232 in combination with a light source 233, the reference mark 212 and the scanner 223 function as a means for determining the position of the lens 206.
This combination of FIG. 2A utilizes the x y scanner 223 to create stereoscopic images of the lens with only a single ccd camera 232. Optical images of the eye 213 and in particular optical images of the natural lens 103 of the eye 213 are conveyed along a path 211. This path 211 follows the same path as the laser beam 210 from the natural lens 103 through the laser patient interface 207, the focusing optics 224, the x y scanner 223 and the beam combiner 222. This combination of FIG. 2A further comprises: a laser patient interface 207, with a reference mark 212; and a light source 233, which could be for example uniform illumination, a slit illumination, or other structured light source designed to enhance 3-dimensional accuracy. The light source, in part, provides illumination of the natural lens of the patient's eye for the purposes of determining the 3-dimensional position of the lens. Thus, either stereoscopic images and/or the information from the camera are sent to a controller and/or computer (not shown in FIG. 2A) for further processing and use in determining 3-dimensional positions of the lens. Stereo images may be generated by commanding the scanner to go to and pause at a nominal left position and then electronically trigger the camera and controller to capture and store the left image; then command the scanner/camera/controller similarly to capture and store right image. This sequence may be repeated in a periodic manner. These left and right images can be processed by the controller to generate the position and shape of the lens. The left and right images can be displayed using a stereo video monitor. Camera images or stereo images may also be used to measure suture geometry and orientation in the patients lens, which can be used to determine the parameters of suture based shot patterns and to align suture based shot patterns to the patients lens suture geometry and orientation. The combination illustrated in FIG. 2A provides 3-dimensional information that can be used to determine the shape of the lens, including the anterior and posterior surfaces thereof. This information can also be used to visualize the structure of the lens, including sutures. Moreover, the information about the lens obtained from the combination of FIG. 2A can further be used in determining the laser shot pattern and laser shot placement with respect to lens shape and/or structure.
FIG. 2 and FIG. 2A are block schematic diagrams and thus the relative positions and spacing of the components illustrated therein are by way of example. Accordingly, the relative placements of these components with respect to one another may be varied and all or some of their functions and components may be combined.
FIGS. 4A-E illustrate the three branched or Y suture geometry in the context of the structures found in the fetal nucleus 415 of the lens. Thus, these figures provide a more detailed view of the structures illustrated as layer 130, which encompasses layer 122 of FIG. 1A. In FIGS. 4A-E the view of the inner layer of the lens is rotated stepwise from the posterior side FIG. 4A to the anterior side FIG. 4E of the lens. Thus, this layer of the lens has three posterior suture lines 401, 402, and 403. This layer also has three anterior suture lines 412, 413 and 414. The anterior suture lines are longer than the posterior suture lines and these lines are staggered when viewed along the anterior to posterior (AP) axis 411. The lens fibers, which form the layers of the nucleus, are shown by lines 404, it being understood that these are only illustrative lines and that in the actual natural layer of the lens there would be many times more fibers present. To aid in illustrating the structure and geometry of this layer of the nucleus representative fibers 405, 406, 407, 408, 409 and 410 have been exaggerated and individually shaded in FIGS. 4A-E. Thus, as the view of the lens nucleus is rotated from posterior to anterior the positions of these representative fibers, there relationship to each other, and there relationship to the suture lines is illustrated.
The length of the suture lines for the anterior side are approximately 75% of the equatorial radius of the layer or shell in which they are found. The length of the suture lines for the posterior side are approximately 85% of the length of the corresponding anterior sutures, i.e, 64% of the equatorial radius of that shell.
The term--essentially follows--as used herein would describe the relationship of the shapes of the outer surface of the lens and the fetal nucleus 415. The fetal nucleus is a bicorvex shape. The anterior and posterior sides of the lens have different curvatures, with the anterior being flatter. These curvatures generally follow the curvature of the cortex and the outer layer and general shape of the lens. Thus, the lens can be viewed as a stratified structure consisting of long crescent fiber cells arranged end to end to form essentially concentric or nested shells.
As provided in greater detail in the following paragraphs and by way of the following examples, the present invention utilizes this and the further addressed geometry, structure and positioning of the lens layers, fibers and suture lines to provide laser shot patterns for increasing the accommodative amplitude of the lens. Although not being bound by this theory, it is presently believed that it is the structure, positioning and geometry of the lens and lens fibers, in contrast to the material properties of the lens and lens fibers, that gives rise to loss of accommodative amplitude. Thus, these patterns are designed to alter and affect that structure, positioning and/or geometry to increase accommodative amplitude.
FIGS. 5A-C illustrate the six branched or star suture geometry in the context of the structure found in the infantile layer of the nucleus 515 of the lens. Thus, these figures provide a more detailed view of the structures illustrated as layer 124 of FIG. 1A. In FIGS. 5A-C the view of the layer of the lens is rotated from the posterior side FIG. 5A to a side view FIG. 5B to the anterior side FIG. 5C. Thus, this layer of the nucleus has six posterior suture lines 501, 502, 503, 504, 505, and 506. This layer of the nucleus also has six anterior suture lines 509, 510, 511, 512, 513, and 514. The anterior suture lines are longer than the posterior suture lines and these lines are staggered when viewed along the AP axis 508. The lens fibers, which form the layers of the nucleus, are shown by lines 507, it being understood that these are only illustrative lines and that in the actual natural layer of the lens there would be many times more fibers present.
The shape of the outer surface of the lens essentially follows the infantile nucleus 515, which is a biconvex shape. Thus, the anterior and posterior sides of this layer of the lens have different curvatures, with the anterior being flatter. These curvatures generally follow the curvature of the cortex and the outer layer and general shape of the lens. These curvatures also generally follow the curvature of the fetal nucleus 415. Thus, the lens can be viewed as a stratified structure consisting of long crescent fiber cells arranged end to end to form essentially concentric or nested shells, with the infantile nucleus 515 having the fetal nucleus 415 nested within it. As development continues through adolescence, additional fiber layers grow containing between 6 and 9 sutures.
FIGS. 6A-C illustrate the nine branched or star suture geometry in the context of the structure found in the adolescent layer of the nucleus 611 of the lens. Thus, these figures provide a more detailed view of the structures illustrated as layer 126 of FIG. 1A. In FIGS. 6A-C the view of the layer of the lens is rotated from the posterior side FIG. 6A to a side view FIG. 6B to the anterior side FIG. 6C. Thus, this layer of the nucleus has nine posterior suture lines 601, 602, 603, 604, 605, 606, 607, 608 and 609. This layer of the nucleus also has nine anterior suture lines 612, 613, 614, 615, 616, 617, 618, 619 and 620. The anterior suture lines are longer than the posterior suture lines and these lines are staggered when viewed along the AP axis 610. The lens fibers, which form the layers of the nucleus, are shown by lines 621; it being understood that these are only illustrative lines, and that in the actual natural layer of the lens there would be many times more fibers present.
The outer surface of the cornea follows the adolescent nucleus 611, which is a biconvex shape. Thus, the anterior and posterior sides of this layer have different curvatures, with the anterior being flatter. These curvatures generally follow the curvature of the cortex and the outer layer and general shape of the lens. These curvatures also generally follow the curvature of the fetal nucleus 415 and the infantile nucleus 515, which are nested within the adolescent nucleus 611. Thus, the lens can be viewed as a stratified structure consisting of long crescent fiber cells arranged end to end to form essentially concentric or nested shells. As development continues through adulthood, additional fiber layers grow containing between 9 and 12 sutures.
FIGS. 7A-C illustrates the twelve branched or star suture geometry in the context of the structure found in the adult layer of the nucleus 713 of the lens. Thus, these figures provide a more detailed view of the adult layer 128 depicted in FIG. 1A. In FIGS. 7A-C the view of the layer of the lens is rotated from the posterior side FIG. 7A to a side view FIG. 7B to the anterior side FIG. 7C. Thus, the adult layer of the nucleus has twelve posterior suture lines 701, 702, 703, 704, 705, 706, 707, 708, 709, 710, 711, and 712. This layer of the nucleus also has twelve anterior suture lines 714-725. The anterior suture lines are longer than the posterior suture lines and these lines are staggered when viewed along the AP axis 726. The lens fibers, which form the layers of the nucleus, are shown by lines 728; it being understood that these are only illustrative lines, and that in the actual natural layer of the lens there would be many times more fibers present.
The adult nucleus 713 is a biconvex shape that follows the outer surface of the lens. Thus, the anterior and posterior sides of this layer have different curvatures, with the anterior being flatter. These curvatures follow the curvature of the cortex and the outer layer and shape of the lens. These curvatures also generally follow the curvature of the adolescent nucleus 611, the infantile nucleus 515 and the fetal nucleus 415 and the embryonic nucleus, which are essentially concentric to and nested within the adult nucleus 611. Thus, the lens can be viewed as a stratified structure consisting of long crescent fiber cells arranged end to end to form essentially concentric or nested shells.
A subsequent adult layer having 15 sutures may also be present in some individuals after age 40. This subsequent adult layer would be similar to the later adult layer 713 in general structure, with the recognition that the subsequent adult layer would have a geometry having more sutures and would encompass the later adult layer 713; and as such, the subsequent adult layer would be the outermost layer of the nucleus and would thus be the layer further from the center of the nucleus and the layer that is youngest in age.
In general, the present invention provides for the delivery of the laser beam in patterns that utilize, or are based at least in part on, the lens suture geometry and/or the curvature of the lens and/or the various layers within the nucleus; and/or the curvatures of the various layers within the nucleus; and/or the suture geometry of the various layers within the nucleus. As part of the present invention the concept of matching the curvature of the anterior ablations to the specific curvature of the anterior capsule, while having a different curvature for posterior ablations, which in turn match the posterior curvature of the lens is provided. Anterior and posterior curvatures can be based on Kuszak aged lens models, Burd's numeric modeling, Burd et al. Vision Research 42 (2002) 2235-2251, or on specific lens measurements, such as those that can be obtained from the means for determining the position of the lens with respect to the laser. Thus, in general, these laser delivery patterns are based in whole and/or in part on the mathematical modeling and actual observation data regarding the shape of the lens, the shape of the layers of the lens, the suture pattern, and the position of the sutures and/or the geometry of the sutures.
Moreover, as set forth in greater detail, it is not necessary that the natural suture lines of the lens or the natural placement of the layers of the lens be exactly replicated in the lens by the laser shot pattern. In fact, exact replication of these natural structures by a laser shot pattern, while within the scope of the invention, is not required, and preferably is not necessary to achieve an increase in accommodative amplitude. Instead, the present invention, in part, seeks to generally emulate the natural lens geometry, structures and positioning and/or portions thereof, as well as build upon, modify and reposition such naturally occurring parameters through the use of the laser shot patterns described herein.
Accordingly, laser beam delivery patterns that cut a series of essentially concentric, i.e., nested, shells in the lens may be employed. Preferably, the shells would essentially follow the anterior and posterior curvature of the lens. Thus, creating in the lens a series of cuts which resemble the nucleus layers of FIGS. 4, 5, 6 and 7. These cuts may follow the same geometry, i.e., shape and distance from the center, of these layers or may follow only a part of that geometry. One example of these shells is illustrated in FIG. 8, which provides a lens 103, a first shell cut 801, a first shell 802, a second shell cut 803, a second shell 804 and a third shell cut 805. The adult nucleus 128 and cortex 113 are also provided. Thus, the term shell refers to the lens material and the term shell cut refers to the laser beam delivery pattern and consequently the placement of the laser beam shots in the lens in accordance with that pattern. More or less shell cuts, and thus shells may be utilized. Moreover, the cuts may be such that they in effect create a complete shell, i.e., the shell and shell cuts completely encompass a volume of lens material. The cuts may also be such that less than a complete shell is formed. Thus, the creation of partial shells, by the use of partial shell cuts, may be employed. Such partial cuts would for example be only a portion of a shell e.g., the anterior quartile, the anterior half, the posterior quartile, stacked annular rings, staggered annular rings, and/or combinations thereof. Such partial shells and shell cuts may be any portion of a three dimensional form, including ellipsoid, spheroids and combinations thereof as those terms are used in their broadest sense that in general follows the contours of the lens, capsule, cortex, nucleus, and/or the layers of the lens including the layers of the nucleus. Moreover, the use of complete and partial shells and shell cuts may be used in a single lens. Thus, by way of illustration of this latter point, the first and second cuts 801 and 803 are annular cuts, while the third cut is a complete cut.
A further use of partial shells is to have the shape of the shells follow the geometry and/or placement of the suture lines. Thus, partial pie shaped shells are created, by use of partial pie shaped shell cuts. These cuts may be placed in between the suture lines at the various layers of the lens. These partial shells may follow the contour of the lens, i.e., have a curved shape, or they may be flatter and have a more planar shape or be flat. A further use of these pie shape shells and shell cuts would be to create these cuts in a suture like manner, but not following the natural suture placement in the lens. Thus, a suture like pattern of cuts is made in the lens, following the general geometry of the natural lens suture lines, but not their exact position in the lens. In addition to pie shaped cuts other shaped cuts may be employed, such as by way of illustration a series of ellipses, rectangular planes or squares.
A further use of partial shells and/or planar partial shells is to create a series of overlapping staggered partial shells by using overlapping staggered partial shell cuts. In this way essentially complete and uninterrupted layers of lens material are disrupted creating planar like sections of the lens that can slide one atop the other to thus increase accommodative amplitude. These partial shells can be located directly atop each other, when viewed along the AP axis, or they could be slightly staggered, completely staggered, or any combination thereof.
In addition to the use of shells and partial shells, lines can also be cut into the lens. These lines can follow the geometry and/or geometry and position of the various natural suture lines. Thus, a laser shot pattern is provided that places shots in the geometry of one or more of the natural suture lines of one or more of the various natural layers of the lens as shown in FIGS. 4, 5, 6, and 7, as well as in the 15 suture line layer, or it may follow any of the other patterns in the continuum of layers in the lens. These shot patterns can follow the general geometry of the natural suture lines, i.e., a series of star shapes with the number of legs in each star increasing as their placement moves away from the center of the lens. These star shaped shot patterns may follow the precise geometry of the natural suture patterns of the layers of the lens; or it can follow the exact geometry and placement of the sutures, at the same distances as found in the natural lens or as determined by modeling of the natural lens. In all of these utilizations of star patterns one or more stars may be cut. The length of the lines of the legs of the star may be the longer, shorter or the same length as the natural suture lines. Moreover, if the length is shorter than the natural length of the suture lines, it may be placed toward the center of the star shape, i.e. the point where the lines join each other, or towards the end of the suture line, i.e., the point furthest on the suture line from the joining point. Further, if the cut is towards the end of the suture line it may extend beyond the suture line or may be co-terminus therewith. Moreover, partial star shaped cuts can be used, such as cuts having a "V" shape, or vertical or horizontal or at an angle in between. These linear cuts, discussed above, are in general referred to herein as laser created suture lines. Moreover, laser created suture lines may be grouped together to in effect form a shell or partial shell.
At present, it is theorized that the use of cuts near the end of the suture lines will have the greatest effect on increasing accommodative amplitude because it is believed that the ends of fibers near the anterior and posterior poles (the point where the AP axis intersects the lens) of the lens are more free to move then the portions of fibers near the equator where there is a greater number of gap junctions which bind fiber faces. At present, it is postulated that it is approximately the last 15% of the fiber length that is most free in the youthful lens with high accommodative amplitude. It is further theorized that fiber layers tend to become bound with age due to a combination of increase in surface roughness and compaction due to growth of fiber layers above. Thus, as illustrated in FIG. 3 a shot pattern 301 is provided to an anterior portion of a layer 302 of the lens. This shot pattern 301 has a contour 303 that follows the contour of approximately the last 15% of fiber length of fibers, represented by lines 304. Thus, the shell cut resembles the shape of a flower. Additionally, the number of petals in the flower shaped shell should correspond to the number of suture lines 305 at that growth layer. Thus, it is theorized that this partial shell cut and/or cuts will have the effect of unbinding the layers and returning the lens to a more youthful increased amplitude of accommodation. Similarly, using partial shells, annular partial shells or planar partial shells in this general area, i.e., the general area at or near the ends of the suture lines, may be employed for the same reasons. This theory is put forward for the purposes of providing further teaching and to advancing the art. This theory, however, is not needed to practice the invention; and the invention and the claims herein are not bound by or restricted by or to this theory.
The use of laser created suture lines, including star shaped patterns may also be used in conjunction with shells, partial shells and planar partial shells. With a particular laser shot pattern, or series of shot patterns, employing elements of each of these shapes. These patterns may be based upon the geometry shown in FIGS. 4-7 as well as the 15 suture line geometry discussed herein; they may follow that geometry exactly, in whole or in part; and/or they may follow that geometry, in whole or in part, as well as following the position of that geometry in the lens. Although a maximum of 15 suture lines is known in the natural lens, more than 15 laser created suture lines may be employed. Moreover, as provided herein, the lens has multiple layers with a continuum of suture lines ranging from 3 to 15 and thus, this invention is not limited to the suture patents of FIGS. 4-7, but instead covers any number of suture lines from 3 to 15, including fractions thereof.
The delivery of shot patterns for the removal of lens material is further provided. A shot pattern that cuts the lens into small cubes, which cubes can then be removed from the lens capsule is provided. The cubes can range in size from a side having a length of about 100 .mu.m to about 4 mm, with about 500 .mu.m to 2 mm being a preferred size. Additionally, this invention is not limited to the formation of cubes and other volumetric shapes of similar general size may be employed. In a further embodiment the laser is also used to create a small opening, capsulorhexis, in the lens anterior surface of the lens capsule for removal of the sectioned cubes. Thus, this procedure may be used to treat cataracts. This procedure may also be used to remove a lens having opacification that has not progressed to the point of being cataractous. This procedure may further be used to remove a natural lens that is clear, but which has lost its ability to accommodate. In all of the above scenarios, it being understood that upon removal of the lens material the lens capsule would subsequently house a suitable replacement, such as an IOL, accommodative IOL, or synthetic lens refilling materials. Moreover, the size and the shape of the capsulorhexis is variable and precisely controlled and preferably is in 2 mm or less diameter for lens refilling applications and about 5 mm for IOLs. A further implementation of the procedure to provide a capsulorhexis is to provide only a partially annular cut and thus leave a portion of the capsule attached to the lens creating a hinged flap like structure. Thus, this procedure may be used to treat cataracts.
It is further provided that volumetric removal of the lens can be performed to correct refractive errors in the eye, such as myopia, hyperopia and astigmatism. Thus, the laser shot pattern is such that a selected volume and/or shape of lens material is removed by photodisruption from the lens. This removal has the affect of alternating the lens shape and thus reducing and/or correcting the refractive error. Volumetric removal of lens tissue can be preformed in conjunction with the various shot patterns provided for increasing accommodative amplitude. In this manner both presbyopia and refractive error can be addressed by the same shot pattern and/or series of shot patterns. The volumetric removal of lens tissue finds further application in enhancing corrective errors for patients that have had prior corneal laser visions correction, such as LASIK, and/or who have corneas that are too thin or weak to have laser corneal surgery.
In all of the laser shot patterns provided herein it is preferred that the laser shot patterns generally follow the shape of the lens and placement of individual shots with respect to adjacent shots in the pattern are sufficiently close enough to each other, such that when the pattern is complete a sufficiently continuous layer and/or line and/or volume of lens material has been removed; resulting in a structural change affecting accommodative amplitude and/or refractive error and/or the removal of lens material from the capsule. Shot spacing of lesser or greater distances are contemplated herein and including overlap as necessary to obtain the desired results. Shot spacing considerations include gas bubble dissipation, volume removal efficiency, sequencing efficiency, scanner performance, and cleaving efficiency among others. For example, by way of illustration, for a 5 .mu.m size spot with an energy sufficient to cause photodisruption, a spacing of 20 .mu.m or greater results in individual gas bubbles, which are not coalesced and dissipate more quickly, than with close shot spaces with the same energy, which result in gas bubble coalescence. As the shot spacing gets closer together volume efficiency increases. As shot spacing gets closer together bubble coalescence also increases. Further, there comes a point where the shot spacing becomes so close that volume efficiency dramatically decreases. For example, by way of illustration, for a 450 femtosecond pulse width and 2 microjoules energy and about a 5 .mu.m spot size with a 10 .mu.m separation results in cleaving of transparent ocular tissue. As used herein, the term cleaving means to substantially separate the tissue. Moreover, the forgoing shot spacing considerations are interrelated to a lesser or greater extent and one of skill in the art will know how to evaluate these conditions based upon the teachings of the present disclosure to accomplish the objectives herein. Finally, it is contemplated that the placement of individual shots with respect to adjacent shots in the pattern may in general be such that they are as close as possible, typically limited by the size and time frame of photodisruption physics, which would include among other things gas bubble expansion of the previous shot. As used herein, the time frame of photodisruptive physics referrers to the effects that take place surrounding photodisruption, such as plasma formation and expansion, shock waive propagation, and gas bubble expansion and contraction. Thus, the timing of sequential pulses such that they are timed faster than some of, elements of, or all of those effects, can increase volumetric removal and/or cleaving efficiency. Accordingly, we propose using pulse repetition frequencies from 50 MHz to 5 GHz., which could be accomplished by a laser with the following parameters: a mode lock laser of cavity length from 3 meters to 3 cm. Such high PRF lasers can more easily produce multiple pulses overlapping a location allowing for a lower energy per pulse to achieve photodisruption.
The terms first, second, third, etc. as used herein are relative terms and must be viewed in the context in which they are used. They do not relate to timing, unless specifically referred to as such. Thus, a first cut may be made after a second cut. In general, it is preferred to fire laser shots in general from posterior points in the laser pattern to anterior points, to avoid and/or minimize the effect of the gas bubbles resulting from prior laser shots. However, because of the varied laser shot patterns that are provided herein, it is not a requirement that a strict posterior to anterior shot sequence be followed. Moreover, in the case of cataracts it may be advantageous to shoot from anterior to posterior, because of the inability of the laser to penetrate substantially beyond the cataract.
Without further elaboration, it is believed that one skilled in the art can, using the preceding description, utilize the present invention to its fullest extent. The following specific embodiments are, therefore, provided as examples of the invention and should be construed as being merely illustrating and not limiting the scope of the invention or the disclosure herein in any way whatsoever.
The following examples are based upon measured lens data and lens data that is obtained by using Burd modeling, which model is set forth in Burd et al., Numerical modeling of the accommodating lens, Visions Research 42 (2002) 2235-2251. The Burd model provides the following algorithm for anterior and/or posterior shape: Z=aR.sup.5+bR.sup.4+cR.sup.3+dR.sup.2+f
The coefficients for this algorithm are set forth in Table II.
TABLE-US-00001 TABLE II a b c d f Anterior (11-year) -0.00048433393427 0.00528772036011 -0.01383693844808 -0- .07352941176471 2.18 Posterior (11-year) 0.00300182571400 -0.02576464843559 0.06916082660799 0.- 08928571428571 -2.13 Anterior (29-year) -0.00153004454939 0.01191111565048 -0.02032562095557 -0- .07692307692308 2.04 Posterior (29-year) 0.00375558685672 -0.03036516318799 0.06955483582257 0.- 09433962264151 -2.09 Anterior (45-year) -0.00026524088453 0.00449862869630 -0.01657250977510 -0- .06578947368421 2.42 Posterior (45-year) 0.00266482873720 -0.02666997217562 0.08467905191557 0.- 06172839506173 -2.42
Additionally, the variables Z and R are defined by the drawing FIG. 9.
Thus, FIGS. 10, 11 and 12 provide cross sectional views of the lens having an outer surface 1001, 1101, 1201 for three ages, 18, 29 and 45-year old respectively, based upon the Burd model and show growth in size along with shape changes with age. The units for the axes on these drawings, as well as for FIGS. 13 to 29 are in millimeters (mm).
EXAMPLE 1, provides for making nested, lens shaped shell cuts. The laser shot patterns are illustrated in FIG. 13, which provides the outer surface 1301 of a 45-year old lens based upon the Burd model. There is further provided a series of nested or essentially concentric shells and shell cuts, which essentially follow the shape of the lens. Thus, there is provided a first shell cut 1302, a second shell cut 1304, and a third shell cut 1306. These shell cuts form a first shell 1303 and a second shell 1305. Shells or partial shells are designed to increase flexibility in the lens by decreasing the strength of nested fiber layers by separating the bound layers, which it is theorized would reduce the structural strength and increase deflection for a given load or force. Thus, although not bound by this theory, it theorized that increasing the deflection of the lens for a given load or zonule force will increase the flexibility of the lens structure and, in turn, the amplitude of accommodation for that same zonule force. Thus, there are provided a nested set of three layers, which essentially follows both the anterior and posterior shapes. Moreover, it being readily understood that for this and the other examples that the shell cut is formed by and thus corresponds to a laser shot pattern.
Thus, the shell cuts in this example are positioned approximately such that the third shell cut 1306 is where 3 suture branches begin forming additional branches, or approximately 6 mm lens equatorial diameter, at the boundary of the fetal nucleus, or the lens at birth; the second shell cut 1304 is where the 6 suture branch layer begins forming additional branches at approximately 7.2 mm diameter, or the infantile nucleus or the lens at approximately age 3; and the first shell cut is where the 9 suture branch begins forming additional branches at approximately 9 mm diameter, or at the adolescent nucleus at approximately age 13.
EXAMPLE 2, provides as an alternative to using a 45-year old lens shape from the Burd model, the actual patient lens structural or shape data may be utilized to customize surgery for each patient. As an example, a 45-year old human cadaver lens, whose shape was measured optically and mathematically fit via the same fifth order function used in the Burd model, yields coefficients unique to the measured lens. The outer cross-section shape of this lens and a shot pattern similar to that of Example 1, but which was tailored to the particular lens of this Example is illustrated in FIG. 14. Thus, there is provided in this Figure an outer surface 1401 of the 45-year old lens. There is further provided a series of nested or essentially concentric shells and shell cuts. Thus, there is provided a first shell cut 1402, a second shell cut 1404, and a third shell cut 1406. These shell cuts form a first shell 1403 and a second shell 1405. It is further noted that any of the exemplary cuts and shot patterns can be implemented via partial or full shells and/or can be implemented via modeled (the Burd model being just one example) or measured lens data.
EXAMPLE 3 provides a shot pattern for cutting partial shells on the measured 45-year old lens, and having an excluded defined central zone. Thus, as illustrated in FIG. 15 there is provided an outer surface 1501 of a 45-year old lens, a central zone 1512, partial cuts 1502, 1504, 1506, 1507, 1509 and 1511. This also provided partial shells 1503, 1505, 1508 and 1510. These partial cuts as shown are part of the same generally annularly shaped. Thus, cuts 1502 and 1507, cuts 1504 and 1509, and cuts 1506 and 1511 are the opposite sides respectively of three generally annularly shaped partial.
EXAMPLE 4 provides a shot pattern for cutting partial shells on the measured 45-year old lens and having both an excluded defined peripheral zone and central zone. Thus, as illustrated in FIG. 16, there is provided an outer surface 1601 of a 45-year old lens, a central zone 1622 and two peripheral zones 1620 and 1621. There is further provided partial cuts 1602, 1604, 1605, 1606, 1607, 1611, 1613, 1615, 1617, and 1618 as well as, partial shells 1603, 1608, 1609, 1610, 1612, 1614, 1616 and 1619. As with example 3 and FIG. 15 these cuts are viewed in cross section and thus it is understood that they are opposite sides of generally annular ring shaped cuts, which essentially follow the shape of the lens and which encompasses the central zone 1622. There are thus 5 partial cuts depicted in FIG. 16.
EXAMPLE 5 provides a laser shot pattern for a finer detailed cutting of the lens to approximate the structural boundaries at 3, 4, 5, 6, 7, 8, 9 suture branches, or the use of six shells. Thus, there is shown in FIG. 17 seven essentially concentric shot patterns 1702-1708, which create seven corresponding shell cuts and which also create six corresponding shells 1709-1714. The outer surface 1701 of a 45-year old lens as measured is also provided in FIG. 17. While this example provides for the creation of six shells, it is understood that the lens contains thousands of fiber layers and that it may be desirable to utilize much greater than six shells and up to hundreds or even thousands, depending on the resolution of the laser deliver system and laser beam parameters.
Examples 6-12 relate to the volumetric removal of lens material in a predetermined shape, based upon a precise shot pattern. Thus, these examples illustrate how refractive change by shaped volumetric reduction may be accomplished. This approach recognizes a limitation of photodissruption laser beam delivery, i.e., that the gas bubbles created are considerably larger then the resultant material void found after all gas bubble dissipation occurs. This can have the effect of causing material voids to be spaced further apart than ideal for high efficiency volume removal. Thus, it is recognized that the closest spacing attainable, depending on detailed laser spot size, energy and pulse width, may provide a low, net volumetric removal efficiency, which is the ratio of achieved volume removal to the volume of material treated. A simple example considers a void size equal to the spacing between voids yielding a nominal 50% linear efficiency, which from symmetric geometry has a 25% area efficiency and a corresponding 12.5% volumetric efficiency of void creation. Thus, by way of example an approach is provided whereby the treatment shaped volume is proportionally larger than desired shaped volume removal to compensate for the low volume efficiency. In other words, if a large shape change with low volume removal efficiency is attempted then a small shape change should be achieved. Other effects such as void shape, asymmetries, void location, tissue compliance as a function of age, external forces and more, may effect the final volume efficiency and experimental validation of volumetric efficiency may be required.
EXAMPLE 6 provides a shot pattern and volume removal to make a negative refractive change, or reduce the power in the crystalline lens by 3 Diopters, using the Gullstrand-LaGrand optical model, which would require the removal of approximately 180 um centrally tapering to 0 over a 3 mm radius. As illustrated in FIG. 18 there is provided an outer lens surface 1801 and a shot pattern 1802 for the desired volume removal. To achieve the full 3 Diopters refractive change directly, the shot pattern would have to remove essentially 100% of the shaded region volume which is extremely difficult due to low volume efficiency found in photodissruption laser beam delivery.
EXAMPLE 7, is based upon dealing with low volume removal efficiency and in this example the assumption that we have a volumetric efficiency of 12.5% or 1/8.sup.th we would treat an 8 times larger volume or 1.44 mm thick to compensate for the low volume efficiency, tapering to 0 over the same 3 mm as shown in FIG. 19, which illustrates a lens outer surface 1901 and a shot pattern 1902. As with the prior examples the shape of the shot pattern is based upon and essentially follows the shape of the outer surface 1901 Of the lens.
EXAMPLE 8 provides a shot pattern to cause a refractive change to increase lens power or reduce hyperopia in patients, where the shot pattern is primarily implemented in the anterior region of the lens. This pattern is illustrated in FIG. 20, which provides an outer surface 2001 and thus shape of the lens and a shot pattern 2002.
EXAMPLE 9 provides a shot pattern to cause a refractive change to increase lens power or reduce hyperopia in patients, where the algorithm is primarily implemented in the posterior region of the lens. This pattern is illustrated in FIG. 21, which provides an outer surface 2101 and thus shape of the lens and a shot pattern 2102. This example further illustrates a shot pattern having a shape is modified to primarily follow the posterior curve of the lens.
EXAMPLE 10 provides a shot pattern to cause a refractive change to increase lens power or reduce hyperopia in patients, where the shot pattern is primarily implemented in the central region of the lens. Thus, as illustrated in FIG. 22, there is provided an outer surface 2201 of the lens and a shot pattern 2202, which provides a volumetric shape. It further being noted that the anterior shape of the lens or posterior shape of the lens or both can be utilized to determine the shape of the shot pattern and/or volumetric shape.
EXAMPLE 11 provides two volumetric shot patterns that follow the shape of the lens surface to which they are adjacent. Thus, as illustrated in FIG. 23, there is provided an outer surface 2301 and thus shape of the lens and a shot pattern having two volumetric shot patterns; a first shot pattern 2302 positioned in the anterior region of the lens and a second shot pattern 2303 positioned in the posterior region, which patterns provide a volumetric shape. Thus, the volumetric shapes to be removed from the lens are located in the anterior and posterior regions of the lens and have a surface that follows the anterior and posterior shape of the lens respectively.
EXAMPLE 12 illustrates a manner in which different shot pattern features are combined to address both refractive errors and those to increase flexibility utilizing a plurality of stacked partial shells, which are partially overlapping. Thus, as illustrated in FIG. 24, there is provided an outer surface 2401 and thus shape of the lens and there are provided partial shell cuts 2402, whose extent is defined by a refractive shape, forming annular rings shaped partial shells 2403. The placement of the partial shell cuts are adjacent the anterior surface of the lens as shown it FIG. 24. The partial shell cuts may similarly be placed adjacent the posterior surface of the lens, in which case they should follow the shape of that surface. Thus, by precisely following the individual shape of the layers within the lens more effective cleaving is obtained.
The shot pattern in the figures associated with EXAMPLES 6,7,8,9,10 and 11 are shown to cut horizontal partial planes whose extent is defined by a refractive shape. It is to be understood that as an alternative to horizontal planes, vertical partial planes or other orientation cuts whose extent is defined by the refractive shape may be used.
Examples 13 and 14 are directed towards methods and shot patterns for treating and removal of cataracts and/or for clear lens extractions. Thus, there is provided a method for the structural modification of the lens material to make it easier to remove while potentially increasing the safety of the procedure by eliminating the high frequency ultrasonic energy used in Phaco emulsification today. In general, the use of photodissruption cutting in a specific shape patterns is utilized to carve up the lens material into tiny cube like structures small enough to be aspirated away with 1 to 2 mm sized aspiration needles.
EXAMPLE 13 provides a shot pattern to create 0.5 mm sized cubes out of the lens material following the structural shape of a 45-year old Burd Model lens. It is preferred that the patient's actual lens shape can be measured and used. Thus, as illustrated in FIG. 25, there is provided an outer surface 2501 and thus an outer shape of the lens. There is further provided a shot pattern 2502 that creates grid like cuts, the end of which cuts 2503 essentially follows the shape of the lens. There is further provided one shell cut 2504, which is integral with the grid like cuts. The sequence of laser shots in the pattern in FIG. 25 may be executed from posterior to anterior, as in most of the patterns disclosed herein, to obtain more predictable results by reducing the variation caused by shooting through gas bubbles. However, it may be desirable to shoot cataracts from the anterior to the posterior for the purpose of choosing the lesser of two undesirable effects. Thus, it may be advantageous to shoot through the gas bubbles, or let them dissipate, rather then shooting through cataractus tissue, which much more severely scatters the light and more quickly prevents photodissruption compared to gas bubble interference. Accordingly, it is proposed to photodissrupt the most anterior sections of the cataract first, then move posteriorally, shooting through gas bubble remnants of cataractous tissue, to the next layer of cataract tissue below. In addition to shooting the laser in anterior z planes then moving posterior, it is further provided to essentially drill down anterior to posterior, which we call the z axis throughout this document and then move in x/y and drill down again.
EXAMPLE 14 provides for a clear lens extraction. In this example the shot pattern of FIG. 25 is applied to a clear lens and that lens material is subsequently removed. In this example shooting from posterior to anterior is desirable.
EXAMPLE 15 provides for a precision capsulorhexis. The creation of precise capsulorhexis for the surgeon to access the lens to remove the lens material is provided. As illustrated in FIGS. 30A-D, there is provided an outer surface 3001 and thus an outer shape of the lens. There is further provided a ring shaped band shape cut 3002 and shot pattern. Thus, the figure shows the cross section view of this ring shaped annular band and accordingly provides for two sides 3002 of the ring. The ring shaped capsulorhexis cuts of 100 .mu.m deep, approximately centered on the anterior lens capsule surface and precisely 5 mm in diameter. Since the lens capsule is approximately 5 to 15 .mu.m thick, it is desirable for the depth of the cut to be typically between 5 and several hundred um, although there is not much penalty for cutting several millimeters. This diameter, however, can be varied between 0.1 mm to 9 mm diameter and the capsulorhexis can be elliptical with the x axis different then the y axis or other shapes. A particular IOL may benefit from and/or may require a particular capsulorhexis shape.
Examples 16 to 17 relate to gradient index modification of the lens. Moffat, Atchison and Pope, Vision Research 42 (2002) 1683-1693, showed that the natural crystalline lens contains a gradient index of refraction behavior that follows the lens shells structure and dramatically contributes to overall lens power. They also showed that this gradient substantially diminishes, or flattens as the lens ages reducing the optical power of the lens. The loss of gradient index with age most likely explains the so-called Lens Paradox, which presents the conundrum that the ageing lens is known to grow to a steeper curvature shape that should result in higher power, yet the aging lens has similar power to the youthful lens. Essentially it is postulated that the increase in power due to shape changes is offset by the power loss from gradient index loss. Examples of the youthful vs old age gradient index behavior is shown in FIG. 31, which provides data taken from the more recent work from the same group Jones, Atchison, Meder and Pope, Vision Research 45 (2005) 2352-236. We can see from this figure that the old lens 3101 has a flat index behavior radially 3102 and the young lens 3103 has continuously diminishing index radially 3104 from approximately 1.42 in the center to 1.38 nearer the outer shells of the lens. Thus, based upon this data it is provided to use the photodissruptive laser in the creation of small voids within the lens fiber material which will then fill-in with aqueous humor fluid which has a lower index of refraction and, via area weighting or volume weighting, decrease the net refractive index of a particular region. Accordingly, if different void densities are placed in nested shell volumes, then this would diminish the average index of refraction of essentially concentric regions in a similar manner to the youthful lens.
EXAMPLE 16 provides a gradient index modification, which has different void densities placed in nested volumes, as shown in FIG. 26. Thus, there is provided a series of nested shot patterns 2602 and a lens outer surface 2601, with each pattern creating an incrementally different void density in the lens material. For example, if a nominal 25% weighting efficiency was obtained in the most densely treated region, filling that volume with 1.38 index of aqueous humor, and the remaining region that was 75% lens material of index 1.42, then the average resultant index of refraction would be 0.25*1.38 +0.75*1.42 or 1.41, which we see from FIG. 31, that would restore the gradient from the center to a 2 mm radius, which is most central optical region for visual function. Thus, FIG. 26 shows a distributed regional treatment of increasing density from the center of the lens to the periphery of the lens.
EXAMPLE 17 provides a gradient index modification that is similar to example 16, except that the area where void density is changed is located further from the outer surface of the lens. This example and pattern is illustrated in FIG. 27. Thus there is provided a series of nested shot patterns 2702 and lens outer surface 2701, with each pattern creating an incrementally different void density in the lens material. Moreover, this figure shows a distributed regional shell treatment that is primarily confined to the nucleus.
EXAMPLE 18 provides for the cutting in relation to suture lines. Thus, cuts along either modeled suture lines, according to Kuzak described suture locations as a function of shell geometry with age and shape, or measured suture lines may be used. The latter being provided by the measuring of patient lens sutures with a CCD camera and aligning suture cuts to the measured locations of suture lines. Thus, the brightest suture lines and or those with the widest spatial distribution likely belong to the deepest layers, and perhaps the initial Y suture branches found in the fetal nucleus. Further, there it is provided to cut Y suture shapes at the lowest layers in the lens and then increasing the number of cuts as the layers move out peripherally. Thus, according to these teachings, FIGS. 28 & 29 shows three different cutting patterns 2801, 2802, 2803 in the anterior portion of the lens that can be done separately or in combination. Thus, FIGS. 28A, C & E shows x-y cuts 2801, 2802, 2803 looking down at the anterior side of the lens. FIGS. 28B, D, and F are schematic representation to illustrate that the star shaped patterns follow the shape of the layer of the lens and do not show the actual cut. FIG. 29 is the combination of the illustrations in FIGS. 28B, D, and F to show their relative positions. It is understood that similar suture cuts can be made in the posterior following the posterior shell curves there, based again on either modeled geometry or measured lens data. There is yet further provided cutting 3,4,5,6,7,8,9,10,11,12,13,14 and 15 branch sutures per Kuszak., cut separately or in any combination.
The components and their association to one another for systems that can perform, in whole or in part, these examples are set forth above in detail. Additionally, it is noted that the functions of the methods and systems disclosed herein may be performed by a single device or by several devices in association with each other. Accordingly, based upon these teachings a system for performing these examples, or parts of these examples, may include by way of illustration and without limitation a laser, an optical system for delivering the laser beam, a scanner, a camera, an illumination source, and an applanator which has reference marks thereon. These components are positioned so that when the eye is illuminated by the illumination source, light will travel from the eye through the applanator to the scanner. In this system the illumination source is movable with respect to the eye to provide varying angles by which the eye can be illuminated.
Similarly, such system may also include by way of example and without limitation a laser, a system for determining the position and shape of components of an eye, a camera, a controller (which term refers to and includes without limitation processors, microprocessors and/or other such types of computing devices that are known to those of skill in the art to have the capabilities necessary to operate such a system), an illumination source, and an eye interface device. In this system the scanner is optically associated with the eye interface device, such that when the eye is illuminated by the illumination source, light will travel from the eye through the eye interface device to the scanner. The scanner is further optically associated with the camera, such that the scanner has the capability to provide stereo pairs of images of the eye to the camera. The camera is associated with the controller and is capable of providing digital images of the eye to the controller; and, the controller further has the capability to determine, based in part upon the digital images provided from the camera, the shape, position and orientation of components of the eye.
Moreover, such systems may also include by way of example and without limitation a system for delivering a laser to an eye. This system would have a laser, a scanner, a camera, an illumination source, an eye interface device, a means for determining the shape and position of components within an eye and a means for directing the delivery of a laser beam from the laser to a precise three dimensional coordinate with respect to the components of the eye, the means for directing the delivery of the laser beam having the capability to direct the beam based at least in part on the determination of the shape and position of components within the eye by the determining means.
From the foregoing description, one skilled in the art can readily ascertain the essential characteristics of this invention, and without departing from the spirit and scope thereof, can make various changes and/or modifications of the invention to adapt it to various usages and conditions.
* * * * *
References
D00000

D00001

D00002

D00003

D00004

D00005

D00006

D00007

D00008

D00009

D00010

D00011
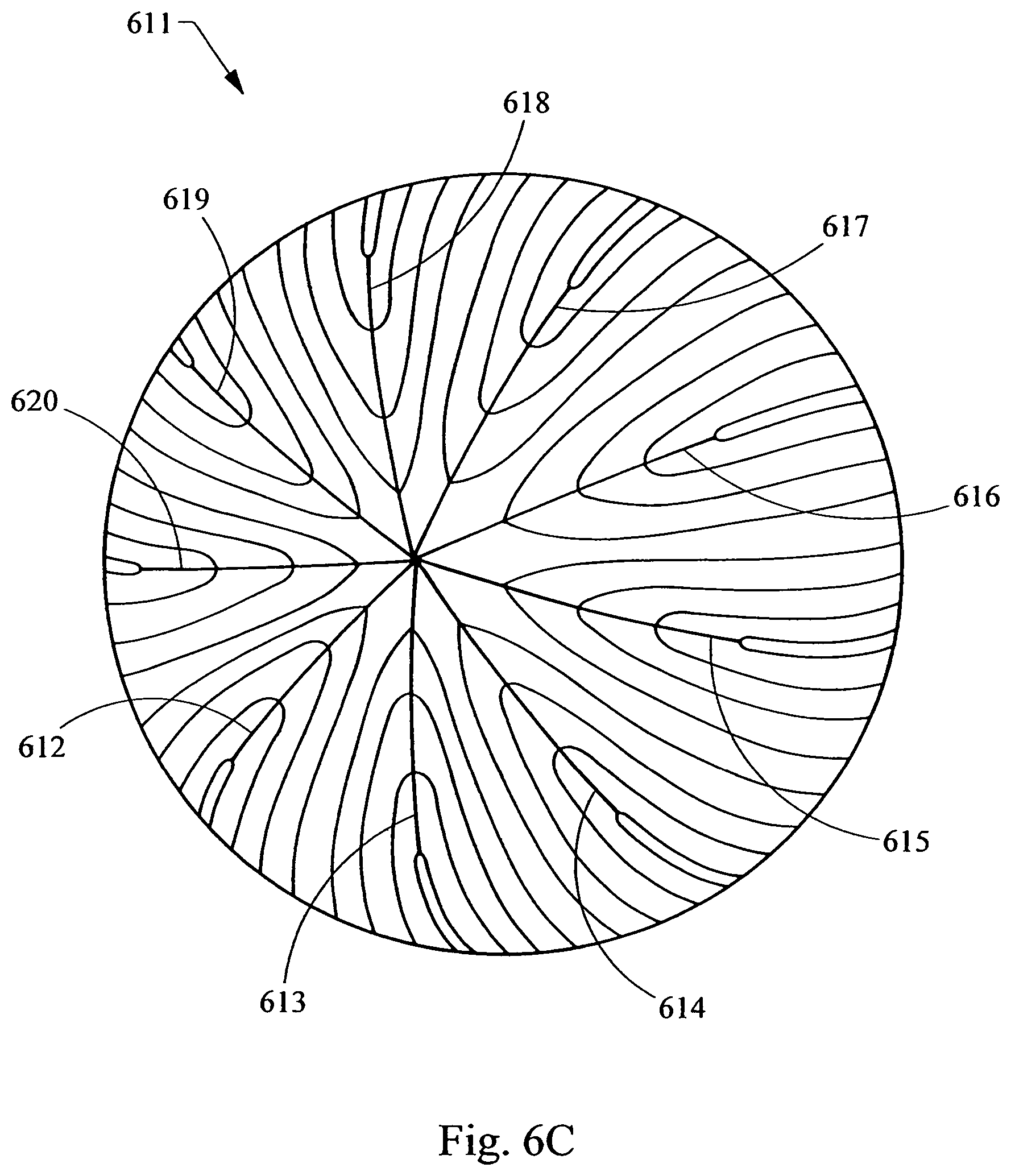
D00012

D00013

D00014

D00015

D00016

D00017

D00018

D00019

D00020

D00021

D00022
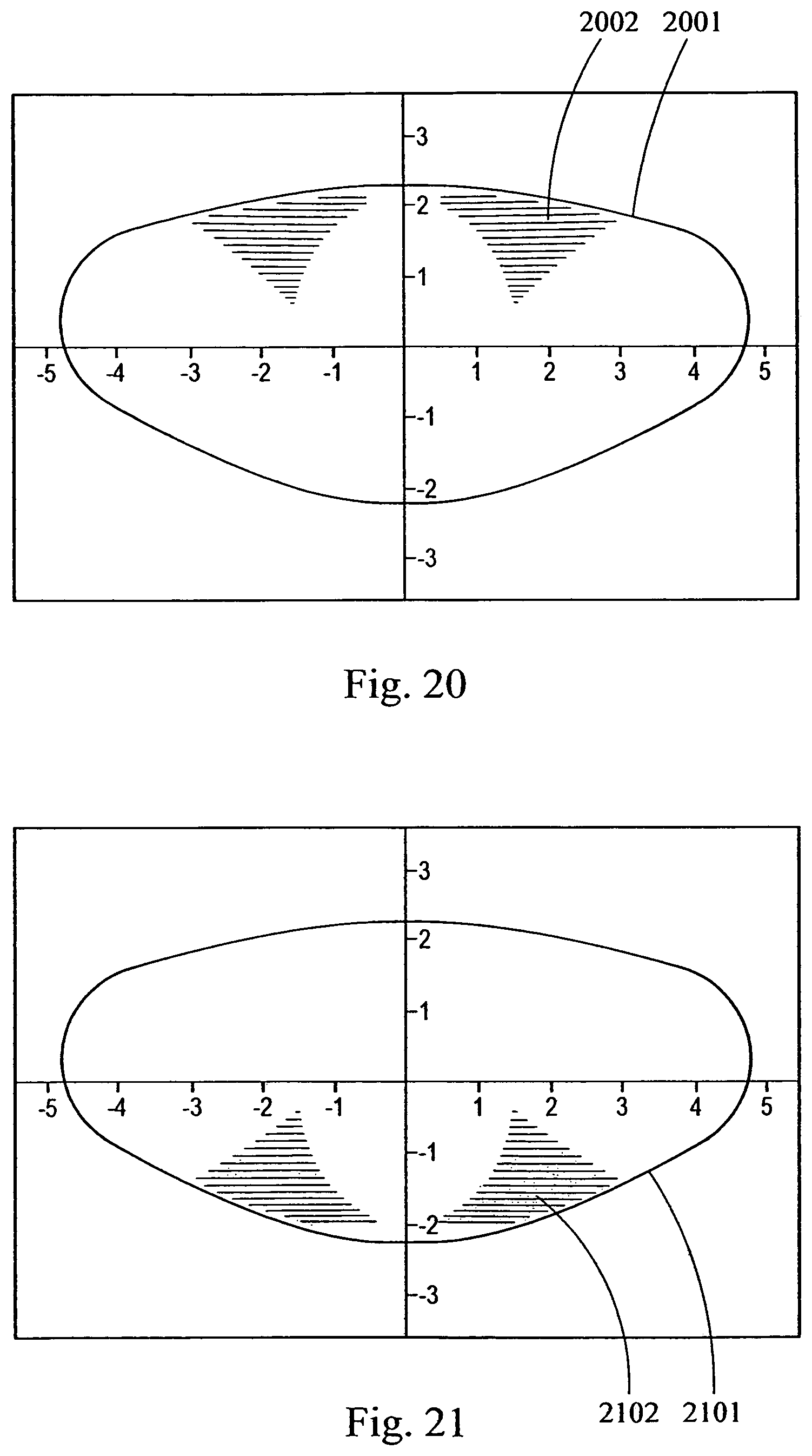
D00023

D00024

D00025

D00026

D00027

D00028

D00029

D00030

D00031

D00032

D00033
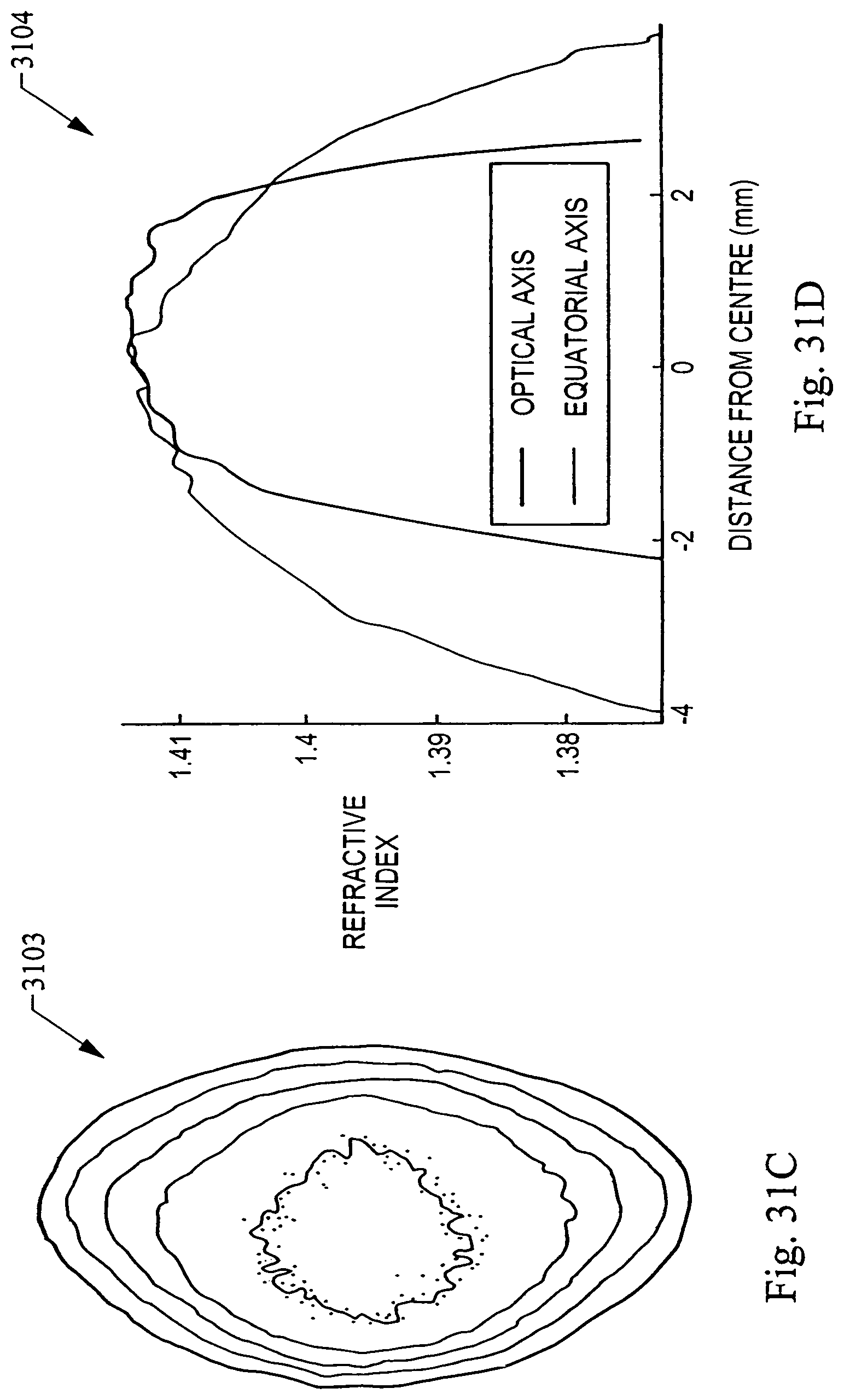
XML
uspto.report is an independent third-party trademark research tool that is not affiliated, endorsed, or sponsored by the United States Patent and Trademark Office (USPTO) or any other governmental organization. The information provided by uspto.report is based on publicly available data at the time of writing and is intended for informational purposes only.
While we strive to provide accurate and up-to-date information, we do not guarantee the accuracy, completeness, reliability, or suitability of the information displayed on this site. The use of this site is at your own risk. Any reliance you place on such information is therefore strictly at your own risk.
All official trademark data, including owner information, should be verified by visiting the official USPTO website at www.uspto.gov. This site is not intended to replace professional legal advice and should not be used as a substitute for consulting with a legal professional who is knowledgeable about trademark law.